Pilot Study to Assess Visual Acuity and Stereopsis in Anisometropic Amblyopic Adolescents and Adults after Contact Lens Correction
Purpose: Treatment of amblyopia in adolescents and adults is considered challenging, time-consuming and often unsuccessful by many health care providers. The aim of this study is to evaluate the success of full refractive correction with soft contact lenses in terms of visual acuity, stereopsis, and visual symptoms in anisometropic amblyopic adolescents and adults.
Methods: 8 subjects (3 females, 5 males; median age of 25.5 years) with unilateral amblyopia caused by anisometropia participated in this investigation. After cycloplegic measurement of refraction, all subjects were fitted with soft contact lenses on a monthly replacement cycle. Distance and near visual acuity as well as local and global stereopsis were assessed five times over the three-month study period. Subjective symptoms were assessed via a questionnaire twice, before and after treatment.
Results: At baseline, median anisometropia (SE) was 2.88 D with a median distance visual acuity of .52 logMAR in the amblyopic eye. A statistically significant improvement in distance visual acuity of the amblyopic eye was measured after three months of contact lens correction (Mdn = .19 logMAR, p = .014). Visual acuity for near improved as well from a median of .32 logMAR to .06 logMAR (p = .002). Global stereopsis improved from a median of 3552" to 135" (p < .001) by the end of the study contact lens wear period. Local stereopsis improved from 300" to 50" (p > .001). Subjective symptoms as assessed by questionnaire did not significantly change before and after treatment.
Conclusion: Contact lens correction alone of anisometropic amblyopia in adolescents and adults resulted in significant improvement of visual acuity and stereopsis for subjects who participated in this study. Larger sample size replication of these results will be important to help establish the efficacy of contact lens treatment of significant long-standing anisometropic amblyopia in adolescents and adults.
Introduction
Good vision is an important factor in a person's development, education, career choice, and practice, as well as orientation and independence. Vision from a holistic perspective is an amalgam of complex developmental sensory and motor processes that are not fully developed at birth. If there are persistent factors that prevent, reduce, or interfere with the acquisition of visual stimuli, the development of the full functionality of the visual system may be negatively impacted. 1–4 If factors interfering with visual development are not recognized and corrected, functional impairment without organic cause may manifest resulting in compromised visual acuity (amblyopia) and impaired binocular vision.2,3,5 Other vulnerable visual functions in amblyopia include accommodation, eye movements and spatial perception. These impairments can affect reading skills and impede academic success relative to non-amblyopes.6–8 It has been documented that with unilateral amblyopia the foveal avascular zone may be altered and the lateral geniculate nuclei may manifest morphologies or atrophies.9–11
A prevalent amblyogenic factor is anisometropia, a refractive imbalance between the two eyes.12,13 When a visual image from the more ametropic eye is significantly less distinct than the image from the contralateral eye, binocularity is compromised. When differential clarity persists, it usually results in a chronic monocular bias for visual information processing and a primary reliance on the contralateral eye for central vision.2,14 Without corrective image equalization between the eyes, the brain learns to ignore or suppress central vision from the amblyopic eye.5 When an amblyope’s contralateral eye has good acuity, there is increased risk for the amblyopia being missed or not detected. This situation most commonly occurs with anisometropic amblyopia when a non-amblyopic eye that is weakly hyperopic or near emmetropic.12,13 Without careful monocular vision screening, the visual deficits present in one eye may be missed and pass undetected into adolescence and adulthood. Population studies show that amblyopia continues to be the leading cause of reduced vision and reduced visual function in the population up to 45 years of age.12,13,15,16 Once the affected individual ages past the traditional treatment age that is believed to be optimal for treatment, therapy is rarely recommended either because the eye-care provider does not believe successful treatment is possible or the required treatment time and effort coupled with a reduced prognosis make success seem unlikely.5,12 In contrast, several studies have documented the existence of visual plasticity with adolescents and adults even well beyond the so-called orthodox treatment-sensitive phase for amblyopia. Studies have documented successful treatment of amblyopia and its associated visual deficits with both adolescents and adults.17–19 To date, few studies have been published using contact lenses as the exclusive treatment modality. Fogt20 and Roberts and Adams21 have shown in their studies of children and adolescents up to 15 years of age that visual enhancement via contact lens correction is possible in anisometropic amblyopia, even after maximal therapy with spectacles and occlusion. The purpose of our pilot study was to determine the extent to which visual acuity and stereopsis could improve by switching from the usual corrective behavior (with or without glasses) to full refractive correction with contact lenses. For this study, it was hypothesized that offering passive contact lens treatment alone would promote subject recruitment, cooperation and optimal study compliance without the requirement of dynamic therapeutic exercises disrupting daily routines of subjects.
Material and Methods
All subjects were recruited from the patient-base of the AugenCentrum Aachen practice. Patients aged 14 years and older with anisometropic amblyopia were considered as eligible candidates. Eight of the 52 patients contacted met all inclusion criteria and agreed to participate in the study. Given the short study duration and the limited number of patient available during the study period, it was not possible to recruit a ‘no treatment’ comparison group. Inclusion criteria specified that both eyes of each subject were healthy and there was no history of eye surgery. Patients with strabismus and eccentric fixation were excluded from the study. Patients with hyperopia, myopia, and astigmatism were included, both with and without correction as well those with a history of childhood occlusion treatment. Patients with > 5.75 D astigmatism were excluded from this study because the lack of availability of contact lenses for that magnitude of astigmatism. The primary outcome factors in this study were the visual acuity (logMAR) of the amblyopic eye for distance and near, plus local and global stereopsis (arcseconds (")). These parameters were measured at five different time points for this study. Following established guidelines and results of other studies, treatment was considered successful with an increase of 0.2 logMAR or more.18,22–26 Subjective changes in symptoms were evaluated using the COVD-QOL (College of Optometrists in Vision Development – Quality of Life) questionnaire. For this study, the Bleything and Landis modified 30-question German translated version was used.27 Anisometropia was defined as a difference in the spherical equivalent of ≥1.0D or astigmatism of ≥ 1.5 D. A person was considered amblyopic if he/she had a distance BCVA of ≤ 0.1 logMAR with a difference of two lines to the better eye. An information sheet, including written informed consent, was signed by each subject (and their parents if younger than 18 years of age) before the start of the study. It also contained information about the collection, handling, and security of subject personal data. Study protocol was in compliance with the German Federal Data Protection Act. A declaration attesting to this was also signed and given to each subject. All subjects participated voluntarily and without financial compensation. All experiments and protocols are conducted following the 1975 Declaration of Helsinki for Experiments on Human Beings, 2013 revision.
Clinical assessment
Each participant’s monocular fixation was measured with the MIT (Macular Integrity Tester; Visus). The Macular Integrity Tester uses subjective localization of the Haidinger’s Brush as a determination of centric or eccentric fixation. Fixation was assessed to rule-out eccentric fixation (study exclusion) as well as to assess the stability of monocular fixation which has been reported as abnormal with some anisometropic amblyopes.6 Cycloplegic, objective refraction (using 0,5 % cyclopentolate hydrochloride, two drops at an interval of 10 min, according to the examiner's usual routine) was done using the auto-refractometer (VD was 12 mm). Automatic 3D measurement was done three times (9 measurements) 45 min after the first drop. All subjects were fitted with the Biofinity® contact lens from Cooper Vision®. This lens was chosen because it is available in a large range of parameters through the XR and XR toric lines. To determine the contact lens correction for each subject, the values of subjective refraction and cycloplegic refraction were considered. Anisometropia and myopia were fully corrected. Hyperopia was either fully corrected or symmetrically under-corrected by no more than 0.50 D. Astigmatism was best-corrected within the available delivery range of the Biofinity lenses. All participants received an information sheet on contact lens handling and hygiene. Contact lenses were prescribed and recommended for daily wear whenever possible. Average wear time was noted at the end of each week for each subject. Visual acuity for distance was measured using a chart projector (M 2000, Müller Wedel) on standardized Landolt rings for each eye as well as binocular. The baseline measurement was done with the habitual correction (glasses or sine correctione). The near visual acuity was tested at 40 cm using a test chart with Landolt rings as well. Evaluation of stereoacuity was measured at a 40cm distance using the original Stereo Fly Stereotest (Stereo Optical Co.) and the original Randot® Stereotest (Stereo Optical Co.). Individuals who could not see the rings in the Stereo Test (Figure 1) and the circles in the Randot® Stereo Test (Figure 2) due to poor stereo vision were tested on the stereo fly (3552") or the larger geometric animal figures (600"). Subjects who could not resolve the geometric animal figures but could perceive “float” on the fly’s wings were listed with default stereopsis of 3552” corresponding to the Titmus stereo fly’s wings. Nearly all study-relevant measures were gathered and recorded by the principal investigator on either Friday, Saturday or Sunday afternoons. The COVD-QOL was administered at the beginning of the study and at the end of the 3-month contact lens treatment period. Paper format questionnaires were provided to completed by all participants under the supervision of the principal investigator.
Statistics
A confidence interval of 95 % and a significance level of 5 % was chosen, α = 0.05. Data was analyzed using IBM® SPSS version 28 and Microsoft® Excel for Mac version 16.51 (21071101). One important prerequisite for correctly planning and performing the statistical analysis of the collected data is the test for normal distribution. With a sample size of n = 8, normal distribution cannot be assumed, but must be tested for. The variables distance and near visual acuity, local and global stereopsis, and COVD score were tested for normal distribution with Kolmogorov-Smirnov and a Lilliefors correction. Since no normal distribution could be assumed for most of the variables after testing and the sample size is very small, only non-parametric tests were used for statistical evaluations and medians with interquartile range were reported instead of means. A Friedman test was run to determine if there were differences between the visual acuity scores for distance when changing from habitual correction to contact lens correction within three months. The Friedman test is the non-parametric alternative to a one-way repeated measures ANOVA. 28 To find out which of the several time points were statistically significant to each other, a post-hoc test with Bonferroni correction was performed. Pairwise comparisons were conducted, and values have been adjusted with a Bonferroni correction for multiple comparisons. An exact sign test was conducted to determine the effect of full contact lens correction on symptoms caused by anisometropic amblyopia assessed with the COVD-QOL. The sign test is used as an alternative to the Wilcoxon rank test to determine if there is a median difference between paired observations at different time points.28

Results
Three female (37.5 %) and five male (62.5 %) subjects between 17 and 51 years of age (Mdn = 25.5, IQR = 26.0) were enrolled in the clinical trial (Table 1). Four subjects (50.0 %) had no correction at the time of enrolling and four of them (50.0 %) wore glasses daily. All eight subjects completed the trial by wearing contact lenses for three months. Lenses were replaced monthly. Visual acuity and stereopsis were examined every month in all patients. There were no missing values. The amount of the correction worn by four of the subjects can be seen in Table 2 (Mdn SEQ = 2.25 D, IQR = 0.75). The four subjects who did not wear glasses at all were recorded as emmetropic. Cycloplegic refraction for the amblyopic eye as well as for the fellow eye were included in the table below to show the differences to the habitual correction and in between the eyes. The median for spherical equivalent of cycloplegic refraction for the amblyopic eye of all eight participants was 4.19 D with a range of 1.13D. The most common form of anisometropia was anisohyperopia (eight subjects) with two of them also had anisoastigmatism (ID 5 and ID 6). Anisomyopia was not present in any of the subjects. It can be seen, that besides the ones with no correction, all participants with glasses as their habitual correction were under corrected. Besides the participant with ID 2, the ones, who wore no glasses, were close to emmetropia (with a maximal amount of + 1.00 D oh hyperopia) in their non-amblyopic eye.

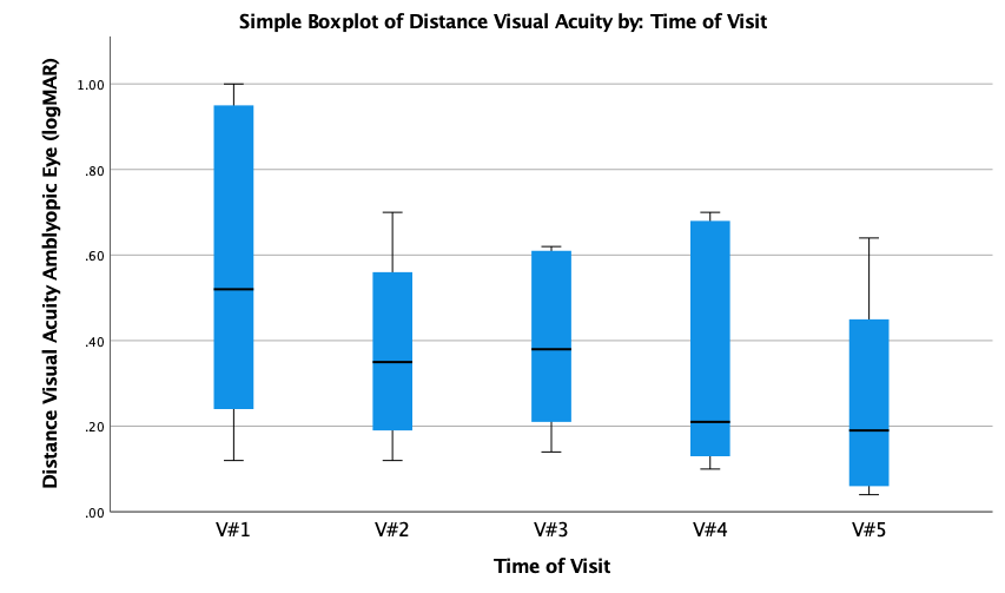
Distance Visual Acuity
As can be seen in Figure 1, the severity of amblyopia within the sample at the beginning of the study is widely scattered, ranging from 1.00 logMAR to .12 logMAR with a median of .52 logMAR. The boxplot for the distance visual acuity, shows, that the visual acuity increases, when changing from habitual correction (V#1) to contact lens correction (V#2) as well as over time. The median changes from .52 logMAR at the first visit to .19 logMAR at the last visit after three months of contact lens correction. Comparing to the first visit, the range of amblyopia amount decreases within the sample with a maximum of .64 logMAR and a minimum of .04 logMAR for the boxplot of V#5. Distance visual acuity of the amblyopic eye was statistically significantly different at the different visits during the trial, χ2(4) = 12.468, p = .014. Post hoc analysis revealed a statistically significant difference in visual acuity between V#1 (VA with baseline correction; Mdn = .52 logMAR) to V#5 (VA after three month of contact lens correction; Mdn = .19 logMAR), p = .009. No other significant differences between any other of the visits from V#1 to V#5 were found. An improvement in distance visual acuity of ≥ 0.2 logMAR was achieved by six participants (75 %).
Near Visual Acuity
As it can be seen in Figure 2, the near visual acuity for the amblyopic eye improved from the first visit with habitual correction to the last visit after three months of contact lens correction. Near visual acuity in the amblyopic eye was better compared to the visual acuity for distance. Starting at the first visit, the acuity ranged from 1.00 logMAR to .00 logMAR with a median of .32 logMAR. After three months of full correction with contact lenses, the acuity improved with a median of .06 and a range from .66 logMAR to.00 logMAR. A Friedman test was also run for near visual acuity. The analysis shows that the distributions of the time points are different. Near visual acuity of the amblyopic eye was statistically significantly different at the different visits during the trial, χ2(4) = 17.452, p = .002. The pairwise comparisons analysis and revealed a statistically significant difference in near visual acuity after Bonferroni correction between V#1 (VA with baseline correction; Mdn = .32 logMAR) to V#5 (VA after three months of contact lens correction; Mdn = .06 logMAR), p = .002.

Global Stereopsis
Global stereopsis improved in all patients comparing V#1 to V#5. Figure 3 shows the boxplots for global stereopsis. Stereopsis of 3552" was recorded if no stereovision could be evaluated with the geometric figures in the test. The dashed line shows the value for the geometric figure in the test with the grossest stereo depth of 600". The figure shows, that at the beginning of the trial, both with habitual correction (Mdn = 3552") and at the initial measurement with contact lenses (Mdn = 1976"), on average no stereopsis could be recorded with the Randot® Stereotest. After three months with contact lens correction, global stereopsis was recorded in all participants (Mdn = 135"). The Friedman test shows a statistically significant difference between the distributions within the trail, χ2(4) = 20.125, p < 0.001. Post hoc analysis revealed a statistically significant difference in global stereopsis between the last visit V#5 and the second visit V#2 with an adjusted significance of p = .034. An even stronger significance can be seen between the sample of V#5 and sample V#1 (p = .005).

Local Stereopsis
Local stereopsis improved in all patients comparing V#1 to V#5. Local stereopsis was reported much better by subjects than global stereopsis. Figure 4 shows that the median local stereopsis improves from time V#1 (Mdn = 300") to V#5 (Mdn = 50"). In addition, already from time point V#2, the distribution within the group is visibly lower compared to the first measurement with the habitual correction. As previously for the other variables, a statistically significant result was obtained for local stereopsis using the Friedman test (χ2(4) = 23.856, p <.001). The post-hoc test indicates three comparison groups for local stereopsis with significance below the p-value of .05. With the adjusted significance score according to Bonferroni, significant results were determined for the distribution of V#5 and V#1 (p < .001) anyway for V#3 and V#1 (p = .007). Also, the measurement after two months (V#4) showed a different distribution than the initial measurement V#1 (p = .016).
COVD-QOL questionnaire
The eight recruited participants, each of whom wore contact lenses for three months, were asked to complete the questionnaire at baseline pre-intervention and post-treatment at the last visit. A negative difference, i.e., a decrease in the score, was seen in four subjects and an increase in score after treatment was seen in three subjects. For one participant, no change could be recorded. A statistically significant change in the median score could not be detected in the COVD-QOL questionnaire due to the change from habitual correction (Mdn = 34.50) to contact lens correction (Mdn = 29.50) after three months (p = 1.00).

Discussion
To evaluate the therapeutic outcome of refractive treatment alone on visual acuity and stereo vision in anisometropic amblyopic adolescents and adults, subjects were fitted with full-correction contact lenses for this three-month long study. Eight subjects were fitted with spherical or toric lenses that were exchanged monthly. This study demonstrated significant improvements in distance and near visual acuity as well as better local stereo vision after three months of contact lens correction in patients who previously wore glasses with under correction, as well as in patients who are not in the habit of wearing previously prescribed glasses. Although local stereopsis was limited at baseline, it was measurable for all but one subject. At the beginning of the study global stereopsis for every participant (except one) was impaired to such an extent that it could not be benchmarked with the available study test tool. Improved local and global two-eyed depth perception was measured at the conclusion of the study. Past research has clearly demonstrated that amblyopia not only causes visual impairment but can also impair motor skills.4,29 These visual functional limitations may influence sports performance/participation, future occupational choices, as well as increase the risk for future accidents.30–32 Therefore, from a public health perspective, amblyopia treatment should be initiated as early as possible in childhood with the understanding that appropriate correction of refractive error is a key foundational element of intervention. Even when anisometropic amblyopia is not detected until adolescence or adulthood, patients should be educated that successful visual treatment is still possible. It has as has been well documented that some degree of visual neuroplasticity persists even into adulthood in adult amblyopes, who have shown significant acuity improvement and perceptual learning in the amblyopic eye following loss of visual acuity in the better eye from either disease or injury.24,33
Evidence suggests that in most cases, untreated long-standing amblyopia and impaired stereopsis in adults can be successfully enhanced by refractive correction alone. With moderate or greater amounts of anisometropia, spectacle lens correction can be problematical for binocularity because of differential magnification and unwanted prismatic artifacts.3,5 In clinical practice, eye care providers and ophthalmologists routinely under-correct anisometropia in order to boost the acceptance of spectacle lens correction or even in some cases under-emphasize the importance of spectacle lens compliance to minimize potential optical/binocular problems.23 However, with contact lens correction differential magnification between the eyes is minimized with far fewer unwanted prismatic effects associated with eye movements. This is because the optical centers of the contact lenses move in concert with the visual axes unlike with spectacle lenses. This study found variable impairments in visual function that varied in severity among the anisometropic amblyopic participants. For example, near visual acuity was better than distance visual acuity for subjects both at the beginning of the study and at the end of the study. There was no statistically significant difference between the amblyopic eye and the contralateral eye for near visual acuity at base line. In contrast, the difference between the two eyes was significant for distance visual acuity. This phenomenon could also be observed with stereopsis. Global stereopsis was only measurable in one subject at the beginning of the study. Only in the last measurement after three months of contact lens correction could global stereopsis be quantified in all subjects. However, for local stereopsis at baseline, seven of the eight patients correctly recognized at least one of the local stereoscopic targets shown. At the end of the study, median results yielded nearly normal local stereopsis of 50". A possible explanation for the difference between the two stereopsis tests may be the monocular detectability of the first three to four targets on the Stereo Fly test. Both clinical stereopsis tests used are somewhat limited for individuals with impaired stereopsis because these tests employ unequal intervals at the beginning end of the measurement scale. The data show that hyperopia is mostly undercorrected and possibly even non-existent myopia is corrected. In amblyopia and anisometropia, measurement with cycloplegia is therefore strongly recommended to better assess the level of ametropia and prescribe adequate correction. If access to diagnostic eye drops is unavailable, collaboration with an ophthalmologist is advised. Full correction is an important element for treatment in amblyopia.25,34
Comparison to other Studies
Visual acuity and stereopsis improvements documented in this study for adolescents and adults with refractive treatment alone are consistent with previous studies.17,18,20,23,25,26 In a relevant Pediatric Eye Disease Investigator Group amblyopia treatment study (ATS), 507 unilateral amblyopic subjects between 7 and 17 years of age were fitted with spectacles. Approximately one quarter of these subjects showed a reduction in amblyopia of about two Snellen lines with optical correction alone.18 Wang et al., studied the effect of refractive correction on 14 subjects (mean age of 13.7 ± 8.4 years) with anisometropic amblyopia. They assessed monocular visual acuity as well as sensory eye balance before and after two months of full correction with glasses. Visual acuity in the amblyopic eye significantly improved (p < .001). Wang et. al., deemed refractive error correction to be a necessary initial treatment, albeit passive.25 Tayyab et al., treated 15 adult anisometropic amblyopes with part-time occlusion in addition to spectacle correction after cycloplegic refractive error measurement. Amblyopia improvement was seen in 73.3% of the cohort. Therapy was considered successful if a visual acuity improved at least 0.5 logMAR.23 The 75% visual acuity success rate with contact lenses documented in our study (at least 0.2 logMAR improvement) is comparable to Tayyab’s spectacle lens correction results. All the listed studies corrected refractive error with spectacle lens glasses. Results from this study indicated significant improvement in visual acuity for distance and near (p = .014, p = .002) as well as significant improvement for both global and local stereopsis (p < .001, p < .001), demonstrating that contact lens correction is also an effective refractive treatment for anisometropic amblyopia.
Roberts and Adams showed that with children (n = 7; age: 3.5-6 years), myopic anisometropia up to 9 diopters can be successfully with contact lenses.21 Fogt fitted non-strabismic children (n = 21; age: 8-15 years), previously “maximally” treated with spectacles and occlusion with contact lenses. Her results indicated that even after occlusion and spectacle lens treatment, contact lenses can further improve visual acuity. According to Fogt, the most likely reason for this further improvement is the elimination of magnification differences between the two eyes.20 Treatment of amblyopia in adolescents and adults via refractive correction leads to successful outcomes both for improved visual acuity and improved binocularity. However, it is important to point out that refractive correction is only a passive treatment and as such it should be considered as an important starting point along with other potential treatment approaches.17 Several new successful treatment approaches have been introduced with adults, including perceptual learning therapy, vision therapy video game play, and near-task oriented therapeutic activities.19,35–37 Occlusion continues to be popular traditional treatment option.23,26,38 The COVD-QOL questionnaire was developed to identify individuals with or at risk for visually-related quality of life complaints27. It can be used to assess the subjective effectiveness of therapies before and after a given intervention. Studies have validated it to be an effective tool for assessing subjective symptoms and impairments of daily living based on symptomology.27,39 It has also been shown that visual symptoms can affect a child’s academic performance; moreover, academic achievement scores have been shown to be inversely related to COVD-QOL questionnaire scores.7
An analysis of our data indicates that a change from the previous habitual spectacle correction or a change from no correction to a contact lens correction derived after cycloplegic refractive measurement results in specific visual function improvement. However, subjective symptoms assessed with the COVD-QOL questionnaire did not improve after contact lens intervention in our study. In all likelihood, contact lenses provoked new symptoms or exacerbated pre-existing symptoms such as dry eye for example. A more specific questionnaire than the COVD-QOL could conceivably better separate contact lens-induced discomfort symptoms from amblyopia-induced QOL symptoms. This information could help idealize contact lens selection for each participant in order to boost long-term contact lens wear acceptance. Amblyopia success is almost always heavily dependent upon lens wear treatment compliance.23 Patients, as reported by Tayyab et al. stated, that after their spectacle lens amblyopia treatment they were able to perform tasks that they did not think they could do before.23 This suggests that subjects' own perception of well-being can be improved by treatment of amblyopia. However, this subjective outcome was not mirrored by our COVD questionnaire results in our contact lens study. Contact lens wear may cause new complaints such as dry eyes, which may lead to progressive deterioration of visual acuity over the course of the day. If it is assumed that the amblyopic eye partially suppresses visual impression and the degree of suppression is negatively correlated with visual acuity and stereo vision, treatment of suppression will lead to higher participation of the amblyopic eye in the visual process.40 It is conceivable that an unfamiliar and possibly a more unpleasant visual impression is created at first, which negatively influences perceived quality of life on the COVD survey. An assessment of overall vision quality and whether future contact lens wear would be preferred might have resulted in a more positive outcome. The study test period may have been too short for full adaptation to the new type of correction along with new viewing habit adoption.
Limitations of the Study
A limitation of this pilot study is that our results are based only on eight participants all of whom were patients at one clinical setting, AugenCentrum. Recruitment of additional patients was unsuccessful for different reasons. With a larger sample size, results may have been different. Given the small number of subjects drawn from our sample of convenience, it is problematic to generalize results from this study to the general population of anisometropic amblyopes. Another limitation was that our sample was too small to differentiate subjects both with and without earlier correction that were included in our analysis. A potential difference in the results between the two groups is quite conceivable and perhaps plausible. Given a larger sample size the "no correction" group would likely demonstrate faster and greater overall visual acuity and stereopsis improvement. More frequent visual symptom assessment over a longer period would also be useful in better understanding the treatment adaptation process. Each subject was previously diagnosed with amblyopia at the AugenCentrum Aachen and best lens corrected acuities had been measured prior to this study at the same clinical location with subjective refraction (Table 1a). An interesting question that was beyond the scope of this pilot study is to explore whether fully correcting anisometropia with size-corrected spectacle lens (to minimize unwanted aniseikonia) would yield similar acuity improvements as contact lenses? Future investigations will be needed to answer this question. In addition, with anisometropia longitudinal studies will be needed to answer the question of long-term and lens wear compliance, visual comfort and whether visual acuity and stereopsis gains are maintained over a longer period.

Conclusion
Results from this pilot study are consistent with earlier published evidence that treatment of adolescents and adults with refractive amblyopia can result in improved visual function. Despite the inherent limitations of this pilot study, it was shown that full refractive contact lens correction derived from cycloplegic refraction can result in improved visual acuity and stereopsis, but not necessarily improved visual comfort or subjective quality of life. From a practical standpoint, even if a refractive amblyopic patient is receiving regular clinical eye care, that patient may be under-corrected and binocularly underserved. Thus, correction of anisometropic amblyopia should not be ruled out regardless of age. Contact lenses can be a good alternative correction tool for enhancing visual acuity and binocularity. Further research on amblyopia treatment is needed, particularly the development and acceptance of evidence-based treatment guidelines for eye-care practitioners.
Conflict of interest
The author declares that there is no conflict of interest in relation to the methods and devices mentioned in this article.
Acknowledgments
I would like to thank Prof. Dr. Anna Nagl and Prof. Dr. Hannu Laukkanen for their constant support. I would like to thank Dr. Katharina Breher and Prof. Dr. Wilhelm Kleppmann for their help with the statistical analysis. I would like to thank Moritz Fanti and the VISUS team for providing the MIT. I would also like to thank my family and friends for their motivation and encouragement.
COE Multiple Choice Questionnaire
The publication "Pilot Study to Assess Visual Acuity and Stereopsis in Anisometropic Amblyopic Adolescents and Adults after Contact Lens Correction" has been approved as a COE continuing education article by the German Quality Association for Optometric Services (GOL). The deadline to answer the questions is 1 October 2023. Only one answer per question is correct. Successful completion requires answering four of the six questions.
You can take the continuing education exam while logged in.
Users who are not yet logged in can register for ocl-online free of charge here.
