Globe Subluxation in the Specialty Contact Lens Practice
Purpose. This report documented the occurrence of globe subluxation (GSL) during the insertion of a scleral contact lens (SL) and described the management of two keratoconus patients, in need of a gas permeable contact lens prescription and experiencing GSL. Furthermore, an anatomical explanation for the occurrence of spontaneous GSL is attempted.
Material and Methods. Two separate case reports of GSL were evaluated and described. In case 1, the patient experienced GSL secondary to insertion of a trial SL and in case 2 the patient had experienced multiple GSLs secondary to Grave’s disease. Different management strategies were taken to help to provide functional vision for these patients. In case 1, the patient was fitted with a smaller corneal gas permeable lens to minimize lid manipulation needed to insert a lens and provide effective correction. In case 2, the patient’s existing Prosthetic Replacement of the Ocular Surface Ecosystem (PROSE) SL was designed to increase vertical lens steepness to tighten the lens fit and minimize the chance of losing the lens during wear.
Results. With the help of the individually fitted contact lenses, it was possible to achieve visual rehabilitation in accordance with the patient’s specific needs.
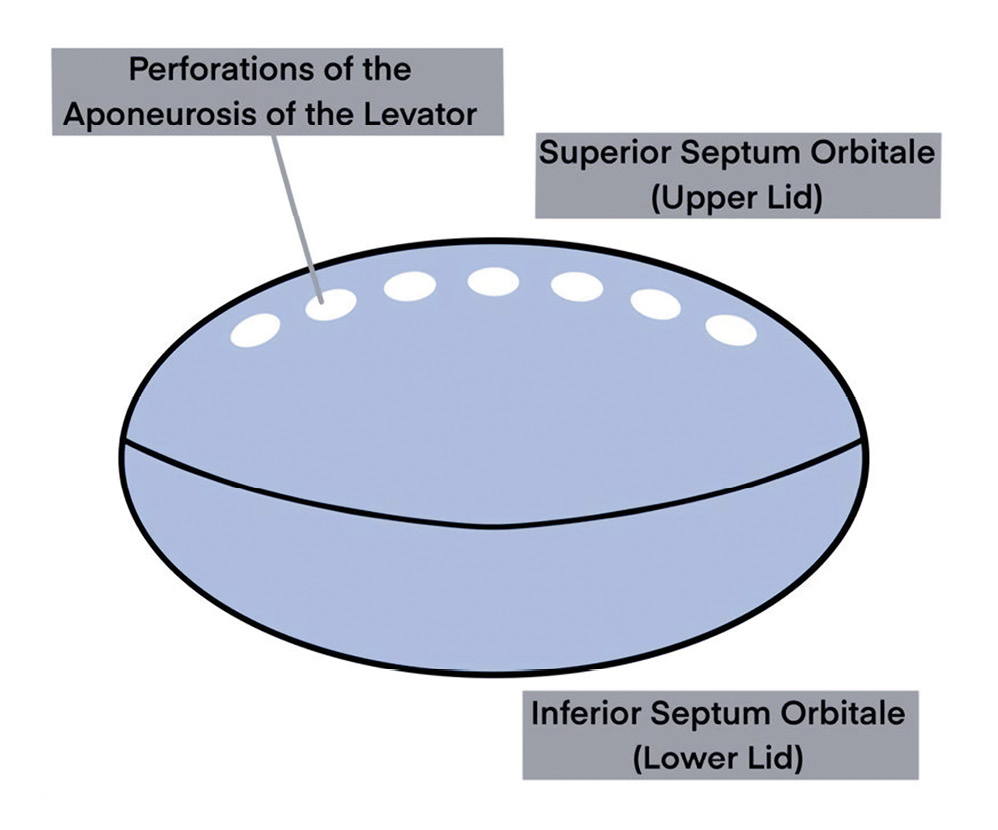
Conclusion. SL are fitted with increasing frequency and tend to require excessive lid manipulation, which may lead to GSL. This small case series demonstrated different lens design and selection maybe utilized to minimize the occurrence of GSL. The superior septum orbitale is perforated several times across the width of the upper lid by the aponeurosis of the levator. This structural arrangement weakens the superior septum orbitale and, postulated here, predisposes the eye to GSL by a herniation primarily of the superior septum orbitale.
Introduction
In some pathological conditions or under certain circumstances the eye may emerge from its normal position in orbit and this occurrence is termed as globe subluxation (GSL) or luxation (Figure 1). Since the globe does not completely depart from the orbit, subluxation is the more accurate term because the word ‘subluxation’ describes a partial dislocation, as opposed to a complete dislocation, to which ‘luxation’ refers.1
GSL can occur due to an abnormal space occupying anomaly or sometimes be a manifestation of a more general pathology.2 Reports in the literature on GSL are limited and often focus on a unique feature of a particular case, such as trauma, obstructive pulmonary disease, floppy eyelid syndrome, proning (chest down positioning), hyperemesis (vomiting) or even voluntary GSL.3,4,5,6,7,8 However typically, case reports do not explain the mechanics of the orbit expelling the globe. Surprisingly, occurrence of GSL in contact lens wearers have not been reported except for one case, describing a habitual soft contact lens wearer experiencing GSL, while inserting a soft lens.9 There have been , no reports of a GSL occurrence during the insertion or removal of a scleral contact lens (SL), which often involves extensive manipulation of the lids. The purpose of this report is to describe the management of two keratoconus patients, in need of a gas permeable contact lens prescription, experiencing GSL. Furthermore, an anatomical explanation for the occurrence of spontaneous global subluxation is attempted.

Methods and Results
Case Reports
This retrospective case series examined 2 patients with different etiologies of GSL. Patients were treated at the University of Houston College of Optometry and Johns Hopkins Wilmer Eye Institute. Access and use of patient records was HIPAA (Health Insurance Portability and Accountability Act) compliant.
Case Report 1
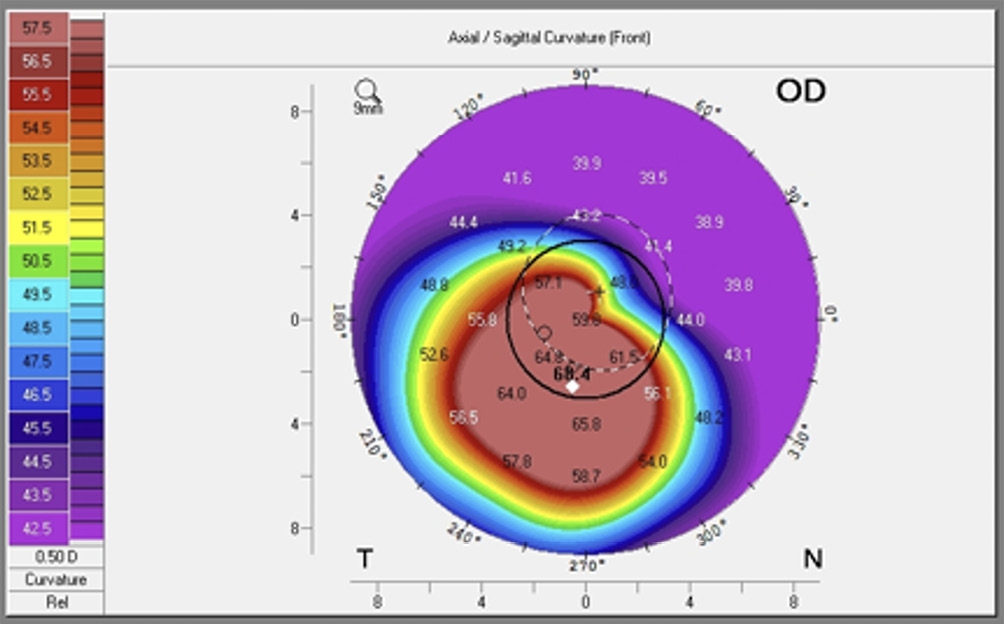
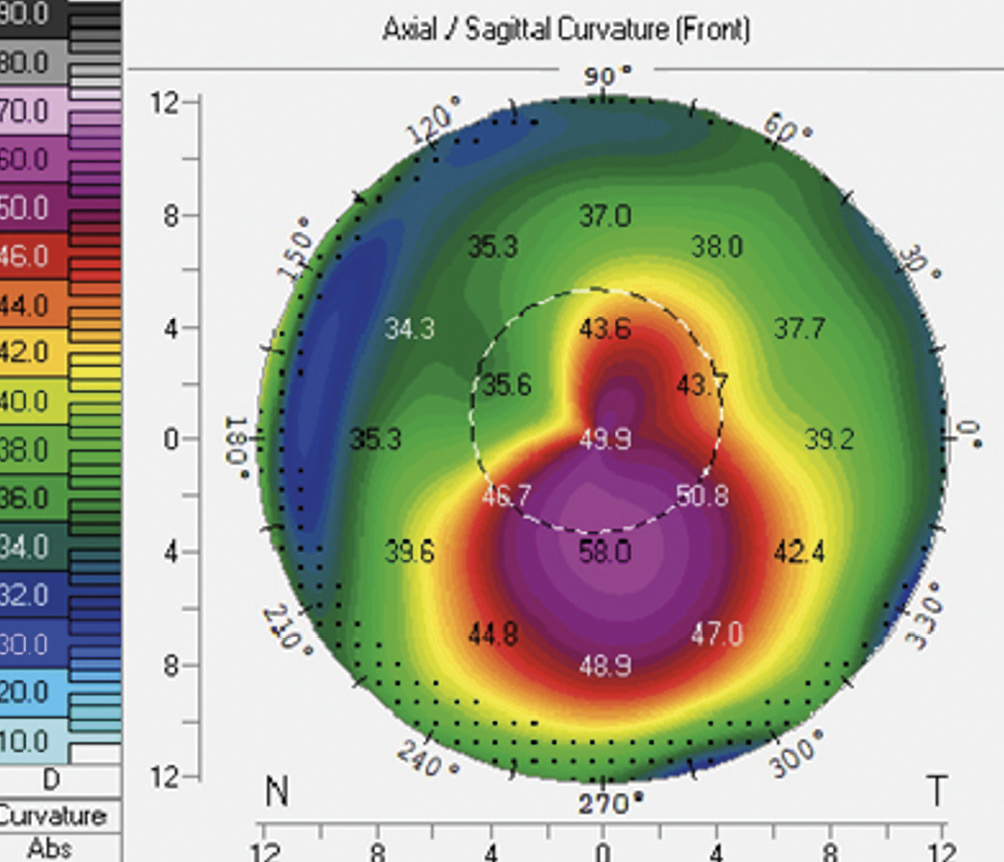
A 31-year old African-American female was referred to the University of Houston, University Eye Institute Cornea and Contact Lens Service for a specialty contact lens fitting due to a history of keratoconus. The patient was first diagnosed with bilateral keratoconus 15 years prior and mentioned a history of excessive eye rubbing. The patient has only worn spectacles and has never tried any kind of contact lens. On the initial examination, best corrected spectacle acuity was 20/100 in her right eye and 20/150 in her left. Biomicroscopic examination revealed positive Vogt’s striae, slight corneal haze and ocular protrusion in both eyes, but negative signs of Fleischer ring and Munson sign. Corneal topography (Pentacam, Oculus, Germany) displayed irregular astigmatism and a classical keratoconus topographic pattern (Figure 2). Keratometry readings were 48.25 @037/58.25 @127 OD and 48.12 @146/59.87 @056 OS and according to the CLEK study classification, both corneas were classified with severe keratoconus.10 Steep corneas made this patient a good candidate for SLs due to significant irregular corneal astigmatism and because a well fitted SL clears without touching the pathological cornea.
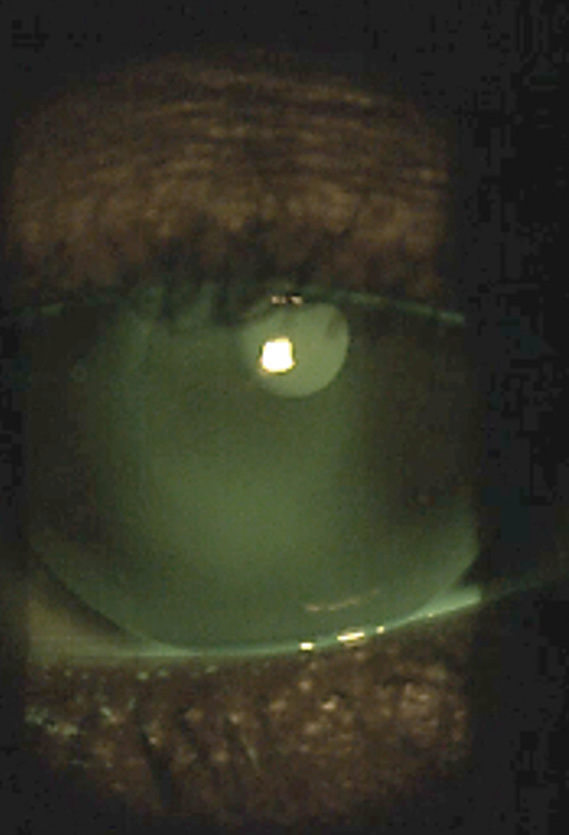
During the initial insertion process of the SL (Zenlens Prolate, Bausch & Lomb, Lancaster, New York, USA) / Prolate / 7.8 mm / −2.00 D / 17.0 mm / 5200 SAG Boston XO (100 Dk/t material) the patient attempted to move her lids out of the way of the cornea and while manipulating the lids, the patient’s lids became entrapped behind the equator of her globe which caused her globe to become displaced forward and subluxed. In an effort to reverse this condition, the patient was gently reclined back on the exam chair. With the use of gravity and lid manipulation, the globe was able to spontaneously return to its normal orbital position. The patient had a recent physical and blood evaluation and denied the presence of thyroid disease.
As a result of this acute instance of GSL, the patient suffered anxiety towards large lenses and the fitting with SLs was abandoned. Since only gas permeable lens designs were able to provide 20/20 vision, this patient was fitted and prescribed a 9.6 mm (Trukone, TruForm, Fort Worth, Texas, USA) / 5.93 Base Curve / −14.12 D / 9. mm Optimum Extra (100 Dk/t material), overall diameter corneal design avoiding excessive lid manipulation (Figure 3).
Case Report 2
A 50-year old African American male was referred to Johns Hopkins University with complaints of decreased vision and evaluation for a Prosthetic Replacement of the Ocular Surface Ecosystem (PROSE) SL. PROSE treatment involves the design and custom fabrication of FDA-approved prosthetic devices for therapeutic use on a daily wear basis. Devices were designed and fabricated using a proprietary CAD/CAM technology to customize the bearing surface of the device haptic to align with the supporting sclera and a transitional and optic portion designed to vault the cornea. The patient had a history of Grave’s disease associated with hyperthyroidism, for which he had been taking Synthroid orally. The patient experienced a history of GSL as a child due to the extent of bulging eyes and, as a result, multiple surgeries were performed on his right eye including an orbital decompression in 1999. The orbital decompression surgery was performed to expand the volume of the orbit by partial removal of the bony orbital rims and fat (Figure 4). This surgery can reduce or reverse vision loss, related to optic neuropathy, prevent ocular surface damage, and relieve orbital congestion.11 In addition, further along in his life, a penetrating keratoplasty was performed in the same eye due to the previously diagnosed keratoconus, intolerance of wearing a contact lens earlier in his life, and extensive presence of corneal scarring.
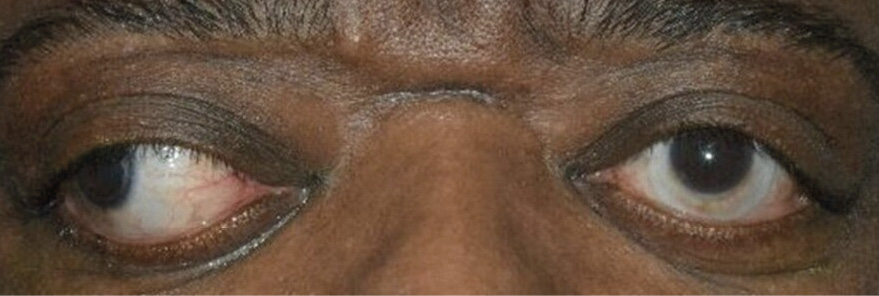

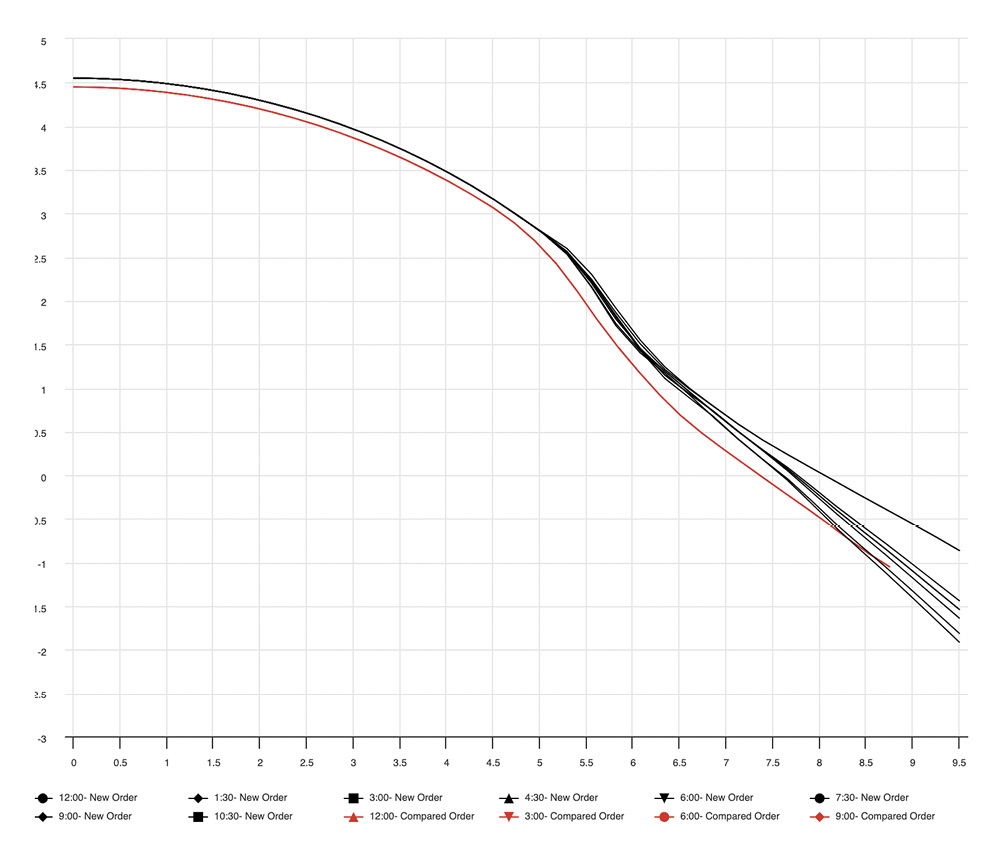
At the one month post-corneal graft surgery he returned for a PROSE evaluation. At his consult visit, it was noted there was significant proptosis and with upper lid manipulation on insertion of the lens, a high possibility of GSL on insertion of the SL. Provider and patient felt the beginning of GSL upon insertion. Fitting was paused for a few minutes, the globe was gently pushed back and in precaution, the PROSE SL was inserted with minimal manipulation of the upper eyelid. The PROSE SL incorporated a large amount of vertical toricity to prevent decentering and to remain stable on the eye. Final PROSE parameters were diameter of 19.0 mm, base curve of 8.00, power of −7.50 with 0.6 eccentricity, material: Boston XO2 (Dk/t 141), and eight quadrants of multiple toricity. The final parameters can be seen in Figure 5 showing the lens peripheral design for Case 2 is much steeper than the normal lens design. Figure 6 shows the topography of the left eye, which had a steepened cornea. By incorporating vertical toricity the lens was able to center while minimizing the chance of it becoming dislodged during wear.
Discussion and Conclusions
The SL is rapidly becoming dominant in the specialty lens field, especially in prescribing for the keratoconic cornea, since this lens design, when fitted correctly, vaults over the cornea and limbus while offering excellent vision and comfort.12 The handling of SL involves significant eyelid manipulations, which may provoke global subluxation in people vulnerable to this ocular complication. The present report describes 2 keratoconus patients experiencing GSL in conjunction with SL management, one case where GSL occurred during the initial diagnostic fitting process and the other was a patient with a history of GSL, that also experienced GSL during the insertion process. The resolution for case one was to prescribe a smaller corneal gas permeable lens requiring less lid manipulation while the second case was resolved by making meridional curvature changes to prevent dislocation or loss of the SL. The present small case series appears to be the first report on GSL occurring in eyecare involving SL.
In case #1 the GSL occurred during trial fitting, when a SL insertion was attempted, and this patient showed great anxiety about continuing with the SL type of lens. However, the patient needed a gas permeable lens design to achieve adequate vision for work and driving. Therefore, she was fitted and prescribed with a 9.6 mm diameter corneal gas permeable lens. In contrast, case #2 already had a preference for SLs and, for this reason, a SL design with a steeper fit was selected to minimize the chance of losing the lens during lens handling or wear. It is clear that an eye vulnerable to GSL may be prescribed with different lens designs depending on circumstances.
Under normal conditions the eyeball and its associated structures are kept in its intended position by the septum orbitale, a connective tissue sheath attached to the internal aspect of the orbital bony rim and at its other end to the peripheral and anterior edge of the tarsal plate of the eyelid.13 Therefore, septum orbitale consists of two portions, one for the superior orbit and upper lid and the other for the inferior orbit and lower lid. It follows that when orbital content is escaping from the orbit the septum orbitale has failed in its function. The structures in view of the observer in GSL is strictly not the globe itself but the conjunctiva overlying the facial sheath wrapped around the globe. This facial sheath, often termed Tenon’s capsule, encloses the globe itself, the muscle cone and ocular nerves and blood vessels. These structures remain attached to the posterior orbital aspects and, therefore, the eye is never completely detached, just dislocated, as is implied by the term ’subluxation’.
The superior septum orbitale is perforated in a number of places across the width of the upper lid by the aponeurosis of the levator (Figure 7). This structural arrangement weakens the superior septum orbitale, especially at its attachment to the lid, which under certain unfavorable circumstances provokes GSL. It is here postulated that global protrusion, as in the small case series presented here, can lead to a herniation of primarily the superior septum orbitale and lead to subsequent GSL episodes.
SLs are being fitted at an increasing rate.14 It is important for SL practitioners to be aware that significant lid manipulation is often required especially for larger diameter SL and awareness of GSL is needed in patients that may have pre-existing proptosis. When GSL occurs in a clinic, practitioners and associated staff must remain calm and try to relax their patient, while also being ready to reconsider their lens selection. The GSL in office occurrence reported here, recovered spontaneously as often is the case by relaxing and reclining the patient. Corneal RGPs are an alternative for scleral lens that should not be overlooked. The fitting process might be more complex compared to scleral lenses, but their handling is easier and, as shown in case #1, these lenses might be a better option for patients at risk for GSL.
Conflict of Interests
The authors declare that there is no conflict of interests regarding the methods and devices mentioned in the article.
