Blunt Force Trauma
Purpose. This case report describes the evidence-based work-up of blunt force ocular trauma that resulted in a zygomaticomaxillary fracture. Sequelae of blunt trauma, management, and referral for surgical consultation will be reviewed.
Material and Methods. A patient presented for an eye examination following a referral from dentistry after receiving a computerized tomography (CT) scan that confirmed orbital fracture to rule out globe injury prior to maxillofacial surgery. The patient underwent a comprehensive dilated examination to evaluate vision, anterior and posterior segment structures.
Results. The examination revealed a sub conjunctival hemorrhage and eyelid edema, with no other signs of ocular trauma. After the comprehensive examination, the patient was educated on the finding of a subconjunctival hemorrhage and was reassured regarding the self-limiting and benign nature of the condition. The patient was cleared for maxillofacial surgery and instructed to return to the clinic for refraction and to rule out any delayed sequelae of ocular trauma.
Conclusion. Blunt force trauma to the eye can cause a host of ocular sequelae that may present as acute or delayed signs and symptoms. These sequelae can be managed by optometrists in hospital and outpatient settings. It is important to be aware of the potential long-term sequelae and how to treat, manage, or refer these patients. Reassurance is important when patients present with ocular signs that appear more alarming than they are. Education is imperative to preventing reoccurrence of trauma and to motivate the patient to remain compliant with the treatment plan.
Introduction
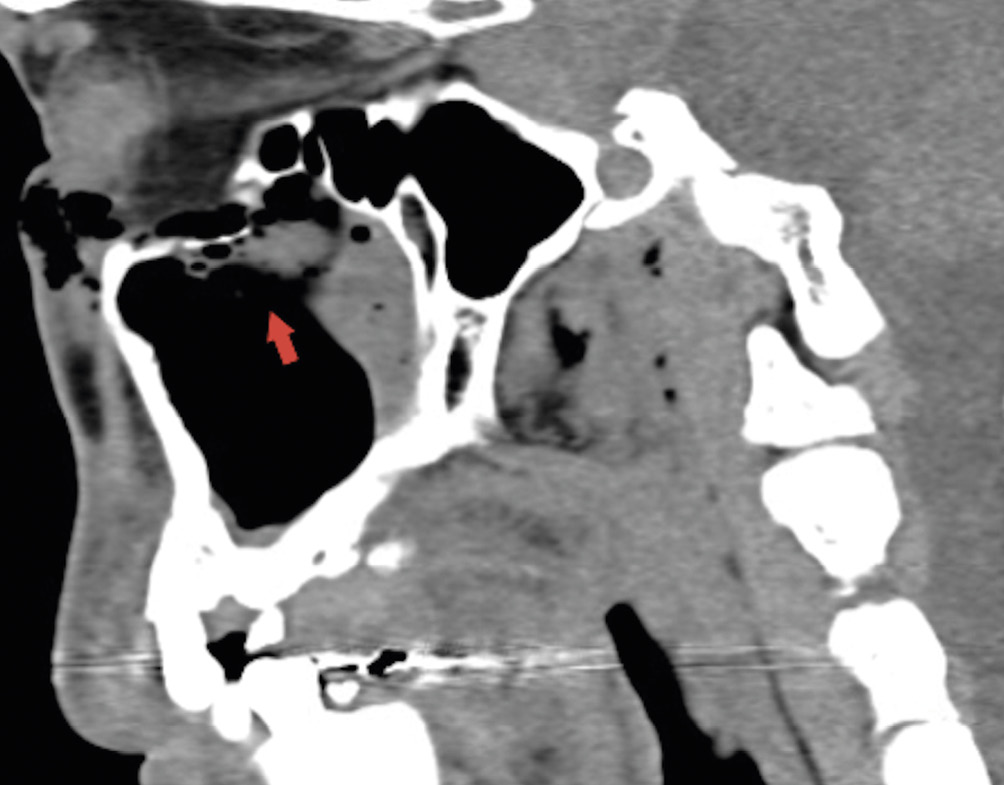
A 41-year-old Black male presented for an evaluation after a physical altercation involving a bodily contact injury five days prior that led to blunt trauma to the patient’s right eye. The patient was referred by dentistry. The patient was diagnosed with a right zygomaticomaxillary complex fracture and requested that optometry rule out globe injury prior to oral/maxillofacial surgery the next day. The CT scan revealed a fracture involving the anterior and posterior wall of the right maxillary sinus with a small amount of fluid and fracture of the floor of the right orbit (Figure 1 and Figure 2). The CT scan revealed no entrapment of the extra ocular muscles. The scan also revealed an undisturbed left maxillary sinus and orbit.
The patient reported pain in upgaze and redness in the right eye. These symptoms presented acutely. Additionally, the patient reported tearing in both eyes as well as longstanding blurry vision in only the left eye. The patient had a history of spectacle wear, but rarely wore the spectacles and did not bring them to this visit. Due to the problem focused nature of the exam, objective refraction, as well as other testing, was deferred to a future follow up visit. The patient had no other pertinent ocular or medical history.
In this case presentation, the evaluation process for trauma is reviewed to rule out urgent and emergent ocular sequelae.

Material and Methods
During the ocular examination, visual acuity was assessed with a projected visual acuity chart calibrated for twenty feet and a standard pinhole occluder. Pupils and extraocular motilities were evaluated with a Keeler transilluminator (Keeler, UK). Intraocular pressure was measured with iCare TA01i (iCare, Finland) handheld tonometer. Anterior and posterior ocular examination was performed with a slit lamp, ninety diopter and twenty diopter Volk lenses (Volk Optical Inc, USA), and Keeler binocular indirect ophthalmoscope (Keeler, USA). Additionally, CT scans obtained prior to the visit were evaluated electronically through our shared electronic health record.
Results
The patient’s best visual acuity was measured as 20/20−2 in the right eye and 20/20− in the left eye, with a pinhole occluder, as the patient did not bring a pair of habitual spectacles at this visit. Pupils were equal in size, round in shape, and equally reactive to light with no afferent pupillary defect in the right and left eyes. Confrontation visual fields were full to finger counting in the right and left eyes. Extraocular motilities were full in the right and left eyes, although the patient reported pain in superior gaze in the right eye. The patient did not report double vision and had no extra ocular muscle restrictions. Intraocular pressure was measured as 10 mmHg and 12 mmHg in the right and left eyes, respectively.
Anterior segment examination revealed normal adnexa with no ecchymosis or crepitus in the right and left eyes. There was mild edema of the upper and lower eyelids in the right eye and trace debris in the lashes of the left eye. Conjunctival evaluation revealed scattered melanosis, diffuse injection and a subconjunctival hemorrhage temporally from six to twelve o’clock in the right eye. The left eye had similar diffuse injection and melanosis, but no subconjunctival hemorrhage. Both corneas were clear with a negative Seidel’s sign. The anterior chamber was deep and quiet in both eyes, with no anterior uveitis. The iris was free of sphincter tears in both eyes. Both lenses were clear and in good position with no acute cataract and there was no Shafer’s sign in either eye.
A dilated fundus examination revealed a clear vitreous, pink, distinct and flat optic nerve head, flat and intact macula with positive foveal reflex, and normal caliber blood vessels in both eyes. The periphery of the right eye was flat and intact 360 degrees, with no holes, tears, or breaks. The periphery of the left eye was grossly flat and intact 360 degrees to the extent seen (due to poor dilation and a subsequent mid-dilated pupil).
The patient was educated on the self-limiting nature of a subconjunctival hemorrhage and mild eyelid edema and that no ocular treatment was necessary besides cold compresses and artificial tears as needed for comfort. The patient was cleared for oral/maxillofacial surgery and was educated to return to the optometry clinic after surgery for refraction and for monitoring of potential delayed sequelae of blunt force trauma.
Discussion
The first provider to see the patient after blunt trauma to the eye should carefully examine the patient to rule out a host of ocular sequelae.1 This includes a thorough history to discuss the mechanism of trauma, the timing, and symptoms. Best corrected visual acuity, and if possible, an objective and subjective refraction, should be performed.1 A reason for any reduction in acuity should be determined, and often warrants a dilated fundus examination and optical coherence tomography focused on the macula. External ocular testing that should be performed includes gross confrontation visual fields, pupil testing and extra ocular motilities.1 Normal pupil responses, specifically the absence of an afferent pupillary defect, would indicate that the patient likely does not have a post traumatic optic neuropathy, although this may be delayed weeks in development after trauma.2 Extra ocular motilities will help reveal if there is any entrapment of soft tissue or extra ocular muscles.1
Blunt force trauma can result in fracture of the bony orbit, as seen in the present case.1 One theory to explain the mechanism of action describes blunt trauma as occluding the orbital aperture leading to increased infraorbital pressure and causing the orbital bones to break at their weakest point.3 Computerized tomography (CT), typically without contrast, is the standard for imaging suspected orbital fractures, especially when it is difficult to clinically examine the patient.1,2 CT scans can help reveal any entrapped muscle and/or soft tissue that may have prolapsed into a sinus and helps aid in estimating fracture size area which is helpful in operative repair. For blunt force ocular trauma, orbital and mid-face scans are the areas of interest, with 1 – 1.5 mm cuts through coronal, sagittal and axial planes. Muscle entrapment, orbital crepitus (a crackling sensation felt and heard typically under the lower eyelid due to trapped air from a sinus), displacement of the globe, and rim notching are some of the indications for a CT imaging referral, if they have not yet had it performed.1
If a floor fracture is present, early surgical intervention is indicated if the patient presents with: CT evidence of muscle entrapment, a large orbital wall defect, associated rim or facial fractures, positive forced duction testing (which indicates entrapped extra ocular muscles), early enopthalmos (inward displacement of the globe) of three millimeters or greater and/or significant hypoopthalmos (downward displacement of the globe), or no clinical improvement over one to two weeks.1
Ecchymosis (bruising) and edema (swelling) of the ocular adnexa are both due to ruptured blood vessels in the eyelids.1 Ecchymosis and edema may be alarming to the patient, but it is often self-limiting in nature. Orbital edema can cause proptosis that may mask inward or downward displacement of the globe due to orbital fracture.1 It is imperative to see the patient back in the clinic for serial exopthalmometry measurements as edema resolves to rule out late displacement of the globe that may require surgery, as mentioned previously. Any lacerations of the peri-orbital skin must be cleaned and covered.1 If the cut is deep, the patient should be referred to an emergency room for stitches or surgery.1
The cornea and conjunctiva should be carefully inspected with sodium fluorescein for abrasions and penetrating injuries.1 Any abrasions should be given an antibiotic eyedrops and monitored daily until re-epithelialization occurs. To determine if there is a penetrating ocular injury, the provider must check for Seidel’s sign. Seidel’s sign is an indication of whether there is aqueous leaking from an open wound.1 There is a positive Seidel’s sign when there is leakage of aqueous. Subconjunctival hemorrhages are due to an increase in episclerous venous pressure that causes capillary leakage.1 The finding is benign, self-limiting, and typically resolves within two-three weeks. Patients can use artificial tears for comfort as needed.1
The anterior chamber must be examined for inflammation by checking for cells and flare with a conical beam in dark illumination.1 Hyphema, otherwise known as blood in the anterior chamber due to rupture of iris and ciliary body blood vessels, is often managed without surgical intervention.1 Patients with a history of endothelial defects, corneal bloodstaining, significant rebleeding, high IOP, or non-clearing hyphema must be referred for surgical intervention that may include paracentesis and anterior chamber washout.1 Gonioscopy should be performed at all follow up visits to check for angle recession.1 Angle recession occurs when the ciliary body muscles are torn, leading to a wider ciliary body band when viewed with gonioscopy.1 Angle recession can lead to glaucoma. If a hyphema is present upon examination, there is a high likelihood that the patient will have a concurrent angle recession.1 The anterior chamber should also be assessed for iris sphincter tears, which can lead to a larger pupil in one eye, known as anisocoria.1 Further, the iris can separate from the scleral spur during blunt trauma, in a condition known as iridodialysis.1
Most commonly, a rosette shaped cataract is expected after ocular trauma due to shock waves.1 Subluxation, dislocation and damage to zonules are other potential sequelae of ocular trauma that can affect the intraocular lens.1 After examining the posterior portion of the lens, the anterior vitreous should also be examined to check for Shafer’s sign.1 Shafer’s sign, also known as tobacco dust, is pigment in the vitreous which is pathognomonic for a break or detachment in the retina.1
Some of the most devastating ocular sequelae occur to the posterior segment. Acute sequelae of ocular trauma affecting the posterior segment include commotio retinae, which is whitening of the retina due to damage to photoreceptors.1 Typically, this is self limiting, but it may result in a permanent scotoma in the patient’s visual field. When commotio retinae occurs in the posterior pole, it is called Berlin’s edema. Traumatic optic neuropathy and rhegmatogenous retinal detachments are often significantly delayed so it is imperative to follow-up with these patients.4,5 Dilated examinations with auxiliary imaging such as retinal nerve fiber layer OCTs and visual fields are necessary to monitor the optic nerve head and retina for atrophy due to traumatic optic neuropathy, which may be delayed if due to a compressive etiology that slowly damages the nerve.1,4 Retinal detachments in patients who have ocular trauma are usually delayed because patients who suffer from ocular trauma are typically younger with well formed vitreouses that take time to liquify and access breaks.5
Extra care should be taken in children to rule out a white-eyed blow out fracture. This is a single or multiple wall orbital fracture in which there is an intact rim with herniation of soft tissue which may include muscle and/or fat.6 This occurs due to children’s flexible bones that act as a “trapdoor” that snap back to their original position after fracture, entrapping tissue along the way.6 Critical signs to look for are a restrictive strabismus in the setting of a white and quiet eye with a history of trauma, oftentimes associated with sports.6 The patient’s presentation to the clinic may be delayed due to the lack of bruising or swelling.6 Some patients may have a vasovagal phenomenon (fainting) and become bradycardic (decreased heart rate) due to the limited mobility.6 It is imperative that children suffering from a white-eyed blow out fracture be referred out for surgery within 1 – 2 days for the best outcome.6
Education of the patient who has suffered from ocular trauma should focus on reassurance and prevention of recurrence.1 Often, ocular trauma can result in signs and symptoms that can be frightening for a patient. Educating the patient that good outcomes are often achieved with compliance with treatment and follow up plans may ease the patient’s concern. Prevention of recurrence is achieved by educating the patient on proper safety recommendations, such as protective eyewear use for sports. Further, compliance with frequent follow ups should be encouraged to monitor for delayed onset sequelae of ocular trauma such as retinal detachment.1,5
Conclusion
Careful examination and evaluation is critical in cases of blunt force ocular trauma. It is advisable to engage in inter-professional communication with the patient’s care team. The eye care practitioner must be careful to perform a thorough examination paying special attention to all possible sequelae of trauma to the eyes. Compassion, reassurance and extensive education is of upmost importance to build trust with the patient and to motivate the patient to be involved and compliant with their treatment and management plan. Long-term observation of the patient’s ocular health and vision is required to monitor for delayed sequelae of blunt force trauma. For further reading and reference, Ocular Injuries Sustained During Blunt Facial Trauma provides a published review on ocular and adnexal injuries due to maxillofacial trauma.7
Conflict of interest
The author declares that there is no conflict of interest regarding the methods and devices mentioned in the manuscript.
