Do MCH prisms change asthenopic complaints when reading?
Purpose. Asthenopic symptoms mostly occur during demanding near-sighted tasks and are related to binocular symptoms (e. g. heterophoria), among others. Correction of symptomatic heterophoria with prismatic glasses is one way to treat the symptoms. This study investigates the effect of wearing a horizontal prismatic correction for 6 months.
Material and Methods. A total of 87 subjects were assigned to a heterophoric prism group (N = 32), a heterophoric control group (N = 31) or an orthophoric control group (N = 24) according to their MCH heterophoria. In the heterophoric prism group, the subjects were prescribed glasses with a prismatic correction for 6 months according to their distance correction; in contrast, the subjects in the heterophoric control group had to wear glasses without prismatic correction for the same period. The effect of the prisms on complaints due to asthenopic symptoms was investigated by comparing the total sum obtained in the CISS questionnaire at the beginning of the study and after 6 months (before and after wearing glasses) for the 3 groups.
Results. A (long-term) prism effect was not apparent in the CISS total score. In both the heterophoric prism group and in the heterophoric control group, the CISS total score increased slightly and non-significantly after 6 months. When considering the heterophoric subjects with an increased CISS score at baseline, a nevertheless slight but non-significant decrease of symptoms was observed. All changes were observed in both the heterophoric prism group and the heterophoric control group. An additional analysis using binocular profiles showed a reduction in symptoms by numbers and specifically for subjects with reduced vergence facility.
Conclusion. Wearing an individual, horizontal prismatic correction had no effect on the overall CISS-score for our test subjects. Further methods that allow a systematic recording of symptoms and optometric parameters are probably necessary to observe an effect. These could be binocular profiles that classify individuals according to their binocular parameters.
Introduction
Asthenopic complaints are usually related to visual problems and those related with the eyes (e. g. headaches, fatigue, burning or aching eyes).1 If the symptoms occur due to working for a long time in front of a computer, tablet or smartphone, they are usually referred to as “digital eye strain” (DES)2 or “computer vision syndrome” (CVS)3. It should be noted that CVS encompasses all problems associated with near vision, regardless of whether they are caused by external factors, such as dry eye, or internal factors, such as binocular problems.1 Attempts have been made to attribute specific symptoms to underlying causes,1 however, as CVS is a collection of different problems with several causes, it is difficult to say what the actual problem is without a comprehensive diagnostic evaluation.4 Asthenopic symptoms, regardless of whether they are caused by devices (i. e. CVS) or analogue, near vision activities, are associated with binocular abnormalities (heterophoria, vergence and accommodation problems), among others 5-7 and play an important role in the clinical optometric examination of patients. When looking closely, as is usually done when reading, for example, the visual system automatically responds with a combination of accommodation, convergence and pupil constriction.8 On the one hand, accommodation focuses the eye on the reading object, on the other hand convergence aligns the visual axes to the point of focus so that the text appears sharp. Under- or over-accommodation is a common cause of asthenopic problems 3 and it has been shown that people who converge more also exhibit more symptoms.9 Currently, between 50 - 75 % of the population suffers from asthenopic symptoms when working in short distances.2 Most of the studies carried out in this context relate to issues when working on a computer or tablet; however, complaints were also observed when digital media were not yet so widespread.10 In this case, test subjects most frequently experienced problems when reading (books or newspapers).
Although the severity of asthenopic symptoms is not directly related to the magnitude of the heterophoria,11,12 the correction of heterophoria is, in addition to the prescription of visual aids for near vision or visual training,5 one of the measures used to reduce the symptoms.13,14 A subjective method for measuring heterophoria is the measurement and correction method according to H.-J. Haase at about 6 metres (MCH for short). Here, both the magnitude of the heterophoria and the correction prism are determined at the same time.15 The MCH method is mainly used in Germany, Austria, the Netherlands and Switzerland to correct heterophoria and the associated visual problems with the use of prismatic spectacle lenses (www.ivbs.org). Interestingly, however, only a few studies show an influence of prismatic corrections on asthenopic problems, whether in the form of an actual reduction of visual issues 16,17 or a positive influence on binocular coordination when reading.18 Therefore, the effect of prisms is still the subject of controversial debate.19
In optometric practice, asthenopic symptoms are usually recorded orally during medical history, even though various questionnaires, such as the Convergence Insufficiency Symptom Survey (CISS)20 have been developed and validated for a more systematic recording and evaluation of such symptoms.20 These questionnaires allow to differentiate between symptomatic and asymptomatic patients and to assign them a specific diagnosis using a scoring system (for example, convergence insufficiency with a CISS total score of more than 21 points).20 In various scientific studies, the CISS questionnaire is also used to record asthenopic complaints that cannot be attributed specifically to convergence insufficiency,21,22 but it is also used to determine the effect of visual measures on symptoms.23 However, there are still many issues related to the CISS questionnaire that remain unsolved. For example, in one of our recent studies we could not find a systematic correlation of the result of the questionnaire with different optometric measurements and binocular parameters.12 For this reason, we took a closer look at the CISS questionnaire 20 and subjected it to a factor analysis.24 We assigned the 15 questions of the CISS questionnaire to 4 independent internal factors, i. e. we were able to group the individual questions into categories that address a superordinate topic area: Category 1 “Eye comfort”, Category 2 “Reading process”, Category 3 “Image quality” and Category 4 “Fatigue”. These categories were similar to those identified by Nunes, Monteiro et al. (2020) for the Portuguese version of the CISS questionnaire.24 These 4 categories showed no systematic correlations with a person’s optometric parameters but were related to aspects of the person's binocular coordination when reading.25
Furthermore, we have recently shown that patients exhibiting problems in binocular coordination could benefit from wearing a prism during 6 months.18 The aim of this article was therefore to investigate asthenopic problems before and after wearing a prism during 6 months. That is why we have compiled further analyses with the aim of gaining a better understanding of the causes of visual problems (CISS totals and the sums of the CISS question categories) in the context of “reading”. Moreover, we have specifically only incorporated the more severe asthenopic problems during reading in an exploratory evaluation section of this article complementing them with considerations that should foster future studies and discussions among professionals.
Material and methods
Test subjects
A total of 87 test subjects (33 men, 54 women) between the ages of 18 and 40 (average: 25.4 years; SD: 4.2) took part in this study. None of the test subjects showed any visual abnormalities: i. e. a monocular uncorrected visual acuity of 0.8 (or more) at 60 cm and showed inconspicuous results for the vertical uncover test and horizontal and vertical cover test and a TNO stereo test (100’’ or better). Patients with strabismus, vertical heterophoria over 1 cm/m or an existing prismatic correction were excluded from the study. Test subjects with horizontal heterophoria detected during the uncover test were not excluded. Each study participant underwent a retinoscopy and a subjective refraction determination (both without cycloplegia) to check their individual correction. The test subjects were also excluded from the study if the measured correction deviated more than 0.5 D (spherical equivalent) from the existing distance correction or if the difference in corrected visual acuity between the two eyes was more than 1 visual acuity level. This procedure guaranteed that all test subjects who participated in the study had good visual acuity and unremarkable binocular vision.
All study participants were informed in writing about the objectives and execution of the study and signed a declaration of consent. The study was conducted in accordance with the Declaration of Helsinki and approved by the Swiss Association of Research Ethics Committees (https://www.swissethics.ch/; project number: 2017-01155).
Measurement of heterophoria
We only selected test subjects with an absolute heterophoria of no more than 4.50 cm/m. Heterophoria was measured using the measurement and correction method according to H.-J. Haase (MCH) at a test distance of 6 m in accordance with the “Guidelines for the application of the measurement and correction method according to H. J. Haase” (see www.ivbs.org for details). The test charts were tested binocularly, whereby some objects were only seen by the right eye or only by the left eye due to the separation by polarisation. All test charts were presented one after the other until a “zero position” was achieved on all tests using prisms. The prism power was then verified using the cross test at close range. The resulting prism corresponds to the heterophoria in cm/m and the correction prism.15
After measuring the heterophoria, the test subjects with an MCH heterophoria between 0.75 and 4.50 cm/m were randomly assigned to a heterophoric prism or to a control group. During the study, the heterophoric prism group received spectacles with the existing distance correction (or a plano correction for emmetropic subjects) and an additional prism corresponding to the individually determined MCH prism. These study spectacles were worn for 6 months. The heterophoric control group also received spectacles with the existing distance correction but without prismatic correction. The remaining study participants with MCH heterophoria between 0 and 0.5 cm/m were assigned to the orthophoric control group and did not receive any spectacles.
Review of regular spectacle wear
All heterophoric test subjects (with and without prismatic correction) were informed verbally and in writing about their expected behaviour during the 6 months of spectacle wear when they were given the study spectacles. They were asked to wear the spectacles for at least 4 hours per day, preferably when working at short ranges. To check compliance, the study participants had to complete an online questionnaire every 2 months in which they indicated how often (days per week) and for how long (number of hours per day) they wore the spectacles. If the minimum duration was not adhered to, the respective test subjects were excluded from the study and were not considered for further measurement
appointments.
Recording the symptoms
The asthenopic symptoms were recorded using a German version of the Convergence Insufficiency Symptom Survey (CISS questionnaire).20 This questionnaire was developed to identify people with convergence-related symptoms in the short range and contains 15 questions on asthenopic symptoms.5 Each question is answered with either never (= 0 points), rarely (= 1 point), sometimes (= 2 points), often (= 3 points) or always (= 4 points); a total of more than 21 points means that the person is conspicuous for convergence-related symptoms in the short range.20 Each of the 87 test subjects completed the questionnaire at the beginning and after 6 months of wearing the study spectacles (recorded time 1 (baseline) and recorded time 2). The first appointment was at the beginning of the study, which also served to check eligibility; the second appointment took place approx. 6 months after the first one. At that point in time the subjects with heterophoria had worn the study spectacles for half a year. The sum of the points of all questions resulted in the CISS total.5 Furthermore, we also determined the individual sums of the question categories on eye comfort, reading process, image quality and fatigue.25 We then compared the change in the CISS total of both heterophoria groups. We divided the procedure in two steps: we first analysed observations for all subjects and then, in a second step, only considered data from participants with more severe symptoms. These were the subjects who had a higher CISS total than the mean value.
The study design
We analysed the questionnaires of the 87 test subjects. The sums of the complaints recorded between the heterophoric prism and control groups and the orthophoric control group were tested using a repeated measures ANOVA to analyse the effect of prism wearing (between the groups and across the two measurement times) or a possible interaction effect (e. g., effect only present in the heterophoric prism group). We used the Shapiro-Wilk test and the Levene test respectively to see if the results were normally distributed and to test the equality of variances. The analyses were performed using the software IBM SPSS Version 27.
Results
In the heterophoric prism group (N = 32), the mean absolute heterophoria (independent of direction) was 2.4 cm/m (SD = 1.1) whereas in the heterophoric control group (N = 31) it was 2.5 cm/m (SD = 1.0).
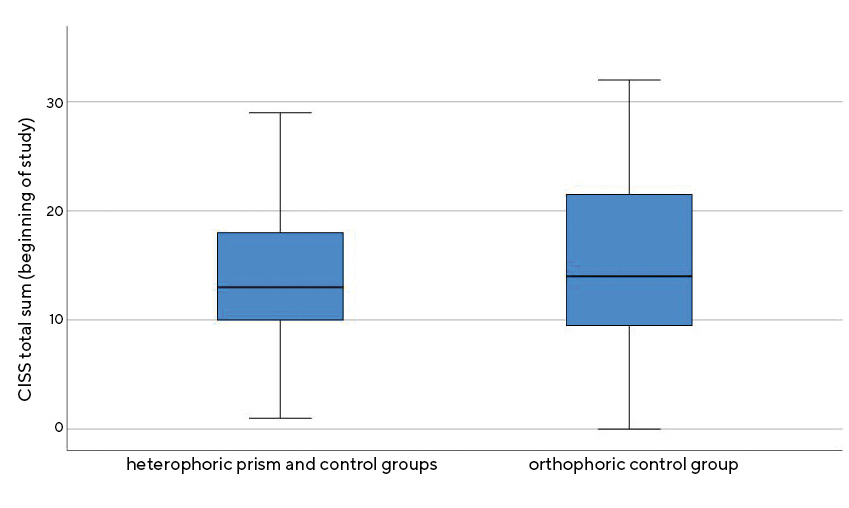
Analyses comprising all test subjects (N = 87) showed that the mean CISS total of the heterophoric study participants (mean value = 13.68 points, SD = 6.33) at the beginning of the study differed only slightly and non-significantly from that of the orthophoric participants (N = 24) (mean value = 15.42, SD = 8.82; t(85) = −1.019; p = 0.311; see Figure 1).
The symptoms at the beginning of the study and after 6 months are shown in Figure 2 and Table 1. In both the heterophoric prism group and the heterophoric control group, the CISS total increased after wearing the study spectacles for 6 months compared to the answers of the questionnaire at the start of the study. In the orthophoric control group, the symptoms slightly declined after 6 months compared to the start of the study. However, these small differences of approx. 1 CISS point were not statistically significant (F = 0.211; p = 0.647).
As the main aim of this study was to investigate the prism effect on asthenopic symptoms, only heterophoric individuals were considered for the subsequent analyses. In clinical practice, prisms are primarily prescribed to symptomatic individuals; therefore, the next step was to analyse how the symptoms of the heterophoric test subjects, who already showed more severe symptoms at the start of the study, would change. Only heterophoric individuals with a CISS total above the mean value of 13.68 points were considered, i.e. all test subjects with MCH heterophoria and a CISS total of 14 or more points (with prism: N = 13, without
prism: N = 16).
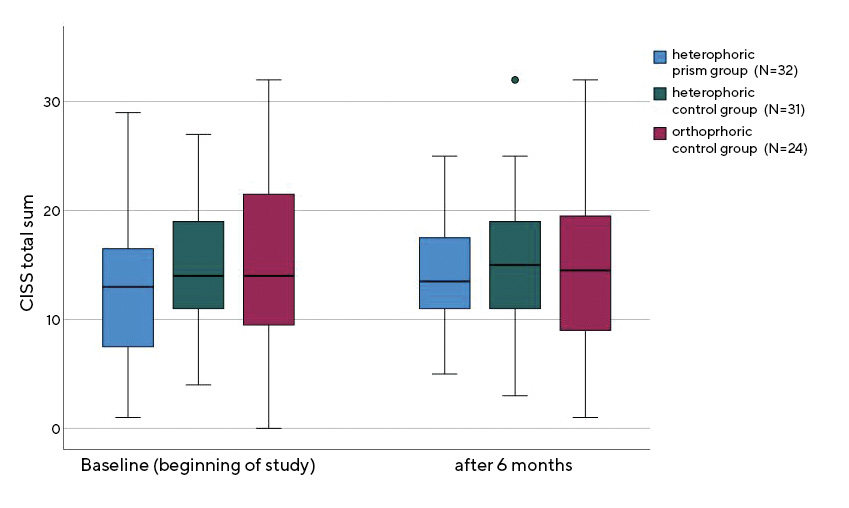
Interestingly, in the subgroup of test subjects with increased symptoms, both the heterophoric prism group and the heterophoric control group showed a tendency to reduce symptoms by almost 2 CISS points after 6 months of wearing the study spectacles (F = 1.409; p = 0.246). It therefore appears that people with more severe symptoms responded to spectacle-wear. In an attempt to determine whether this change could be classified into specific question categories, the four question categories (eye comfort, reading process, image quality and fatigue) were analysed in more detail in a further step.25 A clear tendency towards a reduction in the symptom total was only found for the questions on the reading process (remembering what had been read, feeling of reading slowly, slipping while reading or reading a line several times) (F = 3.891; p = 0.059). This improvement was observed in both groups (heterophoric prism group and heterophoric control group). All other symptom categories showed no significant changes. At the end of the study, the test subjects were asked how satisfied they were with the study spectacles (1 = not at all satisfied; 5 = very satisfied). It was found that the subjects in the heterophoric control group (i. e. without prism) were significantly more satisfied with the spectacles on average (mean value = 4.53; SD = 0.507) than the participants from the heterophoric prism group (mean value = 3.70; SD = 0.907, z = −3.623, p < 0.001).
Further exploratory data analyses
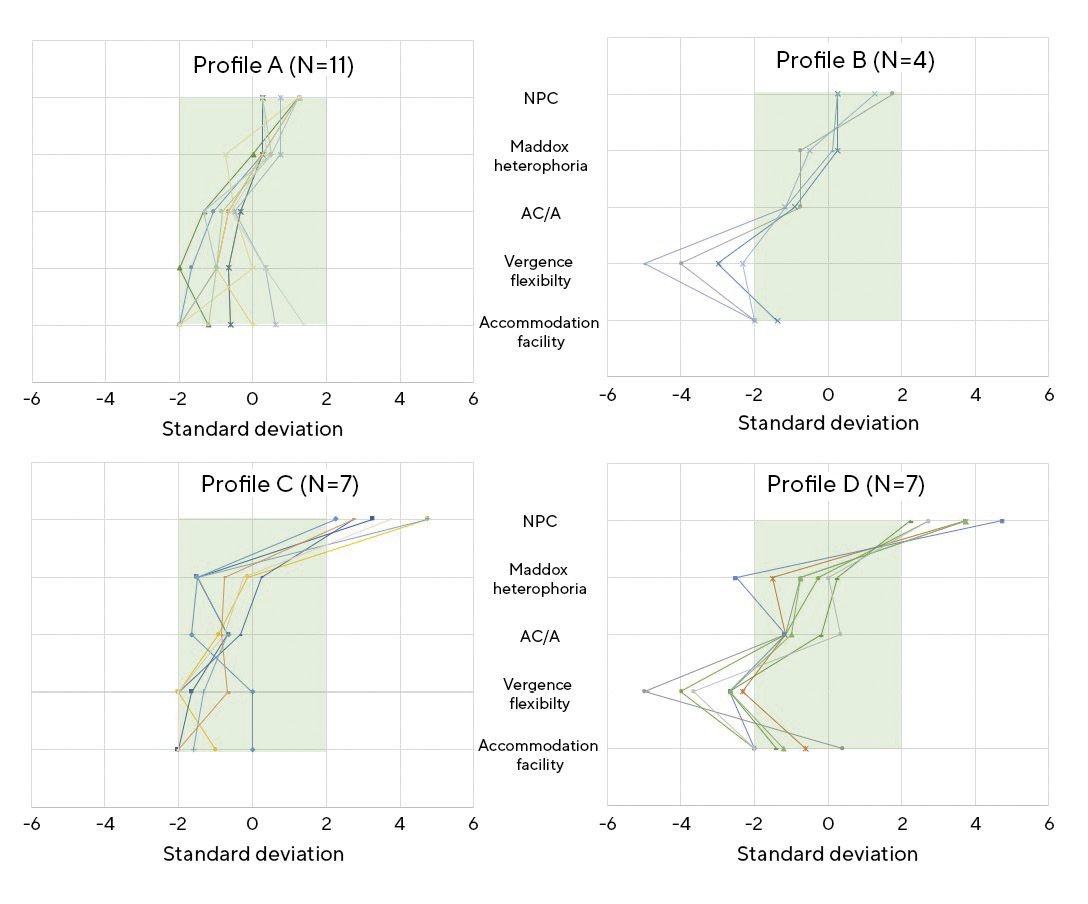
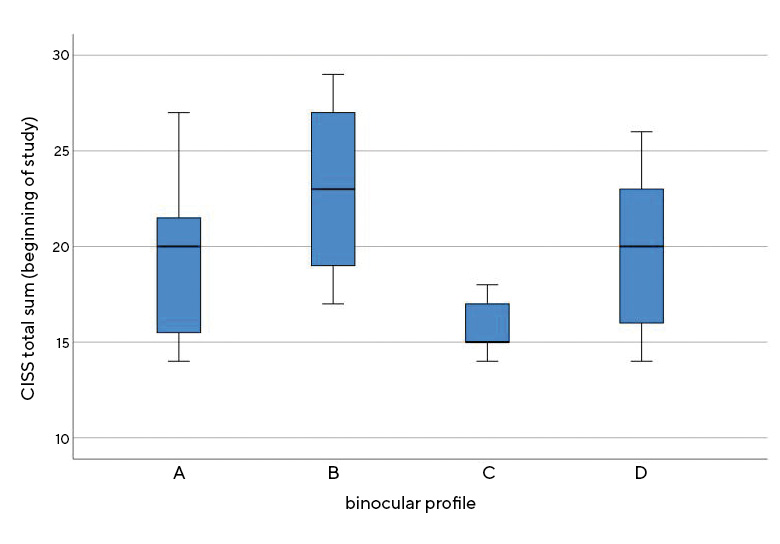
Based on the previous observations, we then used a new approach to create an individual profile for each test subject across several binocular parameters (near point of convergence [NPC], Maddox-Heterophoria, AC/A, vergence and accommodation facility) in comparison to standard values. An alternative categorisation was used for this based on the normal distribution of the data and not on a cut-off value. Similar binocular profiles were grouped together, resulting in four different groups with similar profiles (see Figure 3). We analysed whether each binocular value (NPC, Maddox-Heterophoria, AC/A, vergence and accommodation facility) was within a range of 2 standard deviations around the normal value, i. e. the comparison value (green area). Profile A includes all test subjects for whom all values were within 2 standard deviations of the norm (N = 11).5 Four subjects were assigned to profile B because they showed low vergence facility. Furthermore, seven participants were assigned to profile C because the convergence point was further away from the norm. Finally, profile D includes all individuals who were outside the range of the norm ± 2 standard deviations in both vergence facility and NPC (N = 7). Additionally, the total CISS values were then calculated for these new classification groups (Figure 4). They were highest for profile B (mean value = 23.00; SD = 2.58) and lowest for profile C with mean value = 15.86 (SD = 1.59). This difference between the two profiles showed a clear statistical tendency (F = 2.87; p = 0.057). On average, the CISS total after 6 months was lower for the 4 individuals from profile B (median = 14.50; IQR = 7) than at the beginning of the study (median = 23.00; IQR = 10). A Wilcoxon signed-rank test showed that this improvement was at the limit of significance (z = −1.826; p = 0.068).
Discussion
In this study, we could not detect a long-term effect of the wear of prisms (after 6 months of wearing time) on the CISS total. The mean CISS total of around 14 points is comparable with the results of previous studies.20,26 In addition, it was shown that the CISS total of orthophoric test subjects is similarly high as that of patients with heterophoria. This observation is consistent with other studies, which also found no correlation between heterophoria and asthenopic symptoms.11 Furthermore, 12 out of 24 test subjects without heterophoria also had increased symptoms, i. e. a CISS total of more than 14 points. There are various possible reasons for this:
1. asthenopic complaints have a multifactorial aetiology 4 and heterophoria is only one possible cause; other aspects such as accommodation and vergence parameters, dry eyes, posture when reading or workplace settings could also lead to increased symptoms in orthophoric people. Other parameters would therefore have to be taken into account in a comprehensive (eye) examination to find a possible cause for the symptoms.1,4,7
2. discomfort is subjective, and each person has an individual scale. For example, a person who rarely gets tired when reading may experience a sudden, sporadic fatigue when looking at nearby objects very annoying, in contrast to a person who has become accustomed to it to a certain extent and therefore classifies the discomfort as milder.27
Based on these considerations, primarily heterophoric test subjects were thus analysed and discussed.
All heterophoric study participants (prism group and control group) had similar CISS totals at the beginning of the study. The hypothesis was that, after wearing a prism for 6 months, the heterophoric prism group would exhibit a greater reduction in CISS totals compared to the heterophoric control group. Prismatic corrections are used for symptomatic heterophoria to bring the binocular system into the resting position and thus reduce symptoms.5,15,28 However, no significant change in this respect was observed after 6 months. There are hardly any studies that have investigated the effect of prisms for correcting heterophoria on asthenopic symptoms. Scheiman, et al. (2005) investigated the effect of base-in prisms for the correction of symptomatic convergence insufficiency in children and observed a significant improvement in the CISS total after wearing the prismatic correction for 6 weeks, but found no difference between placebo and prism correction.29 Teitelbaum, Pang, & Krall (2009) studied a novel progressive lens design in individuals with convergence insufficiency in which distant prisms increased at near distances. All subjects wore both the prism and the placebo spectacles over a period of 3 weeks. The visual complaints (CISS total) were reduced significantly more by wearing the prismatic glasses than by wearing glasses without prisms.17 Both studies had shorter wearing periods than in the present study; it is possible that an effect was observed that was present at the beginning of the wearing phase but was no longer detectable after 6 months.
As prismatic corrections are generally only prescribed to symptomatic individuals 15,28 heterophoric patients with a CISS total of more than 14 points were considered for further analyses. This showed that the CISS total decreased by 2 points after 6 months. In addition, a reduction in the sum of the question category on the reading process was observed at the second recording date. However, these changes were similar for the prism and control groups and therefore cannot be attributed to the effect of wearing prisms. Thus, even when looking at the test subjects with more severe symptoms, no correlation between the change in symptoms and the wearing of a prismatic correction could be established.
It is possible that the long-term prism effect on the CISS total could not be demonstrated because it was too small, too unstable or too global, or because the available MCH heterophorias (max. 4.50 cm/m) were too small. However, other previously published analyses have shown that a 6-month prism wearing phase has a positive effect on the binocular vision while reading, as the objective fixation disparity was reduced and the cooperation of the eyes improved, even with MCH heterophorias up to 4.50 cm/m.18 Prisms can therefore have a positive effect on the visual system, they just do not appear to be directly reflected in the patients’ symptoms. Complaints are generally highly subjective and are therefore subject to a high degree of variability, even within a single person.27 The present study did not specifically examine people with severe symptoms. For people with significantly higher CISS totals, a stronger change could possibly be observed regarding possible symptoms. Other explanations for the lack of effect could be that an alternative method for determining heterophoria would be more suitable than the MCH, as it has been shown that subjective fixation disparity at short distances (measured with the Mallett Fixation Disparity Test) correlates with symptoms.30 In addition, MCH is controversial, as there is little scientific evidence on the actual theoretical background of the method.31 On the other hand, the CISS questionnaire, which was developed to identify convergence insufficiency, may not be suitable for recording asthenopic symptoms in general, even though the CISS questionnaire is used in different ways 22,26 and a significant improvement in symptoms, for example by wearing yellow lenses, has been observed in children using the CISS questionnaire.23 Further research is needed to establish the relationships between optometric parameters such as heterophoria and asthenopic symptoms, being one of the biggest challenges to find suitable methods to capture both the optometric parameters and the symptoms.
When considering the effect of prismatic correction on asthenopic symptoms during reading, no clear, significant improvement in CISS symptoms was observed after wearing a prism for 6 months. It was found that the CISS total of orthophoric test subjects was similar to that of people with heterophoria. Furthermore, it should be questioned whether symptoms recorded in a written questionnaire provide a valid basis for clinical optometric decisions,26 since the observations showed a tendency for symptoms to increase in all participants, which is certainly due to the survey method. Studies show that symptoms tend to be more severe when, on the one hand, they are based on memory 32 and, on the other, when they are recorded using a list (as is the case with the questionnaire).33
Ultimately, however, a reduction in symptoms was observed in study participants with more severe symptoms after 6 months, irrespective of wearing a prismatic correction. This reduction was also observed for specific questions relating to the reading process.
The study results also show that heterophoria is apparently not the only cause of asthenopic symptoms. During the study, an exploratory approach was used to create individual binocular profiles using several optometric parameters and to group the test subjects with similar profiles. Certain trends in terms of symptoms were observed: the CISS totals differed in the different profiles, and the people from profile B showed an improvement in symptoms after 6 months, although the comparisons were not significant due to the small sample. These are certainly preliminary observations to explain asthenopic symptoms; however, more research with a larger sample is needed to confirm these observations in this context.
Ultimately, the available CISS results are consistent with the subjective feelings of the test subjects: all heterophoric participants who already wore glasses before the study (21 people) were asked whether they felt more comfortable with their private glasses or with the study glasses. Of the 11 people who wore the prismatic study glasses, only 3 stated that they preferred the study glasses, all others felt more comfortable without prismatic correction. A satisfaction survey was conducted at the end of the study for all test subjects, regardless of whether they wore glasses before the study or not, which showed that those in the heterophoric control group (i.e. without prismatic study glasses) were generally more satisfied with their study glasses than those in the heterophoric prism group.
The present study addresses a secondary question of a larger study, the results of which have already been published.12,18 For this reason, the study design was not optimised for the influence of prismatic corrections on asthenopic symptoms during reading. Among other things, this meant that only minor heterophoria was investigated and the study participants were not selected based on their symptoms. It must therefore be recognised that the present results cannot be applied to all typical cases in optometric practice (e.g. patients with severe symptoms). However, contrary to a widespread assumption, it was shown that prism effects are not directly and immediately reflected in a reduction in asthenopic complaints, even if it has already been shown for the same sample that there are measurable positive effects in binocular coordination.18
To conclude, it should be noted that the selected CISS questionnaire was originally developed with a different goal. Even though other studies have shown that it can be used for other purposes,21,22 it cannot be ruled out that a different questionnaire variant would have proven more effective for recording asthenopic symptoms while reading. Finally, it should be noted that heterophoria was determined using the MCH, since it is the most common method for qualifying and quantifying heterophoria in Germany, Austria, the Netherlands and Switzerland, although there may be more suitable methods for this.
Conclusion
At first glance, we could not establish any positive effect of horizontal prismatic corrections on the CISS total after wearing prisms for 6 months. Nonetheless, we could observe certain tendencies towards a change in the symptoms mentioned after this time. However, these changes were similar in the heterophoric prism and control groups. The systematic recording of symptoms is challenging due to multifactorial causes and requires tools with high sensitivity and specificity. Furthermore, methods for the systematic recording of abnormalities and problems in binocular vision are also necessary in the field of optometry; one of which was presented in this publication. This approach can and should be further researched in future studies to be able to better explain the complexity of asthenopic symptoms in the near future.
Conflict of interest
The authors have no conflict of interest regarding the methods and devices mentioned in this article. This study was funded by the Swiss National Science Foundation (SNSF; grant no. 320030_172965) and financially supported by the International Association for Binocular Vision (IVBS) for the purchase of spectacle frames and lenses.
555-565.
Preliminary report: prescription of prism-glasses by the Measurement and Correction Method of H.-J. Haase or by conventional orthoptic examination: a multicenter, randomized, double-blind, cross-over study. Strabismus, 9, 17-27.
for Presbyopes with Convergence-Insufficiency. Optom. Vis. Sci., 86, 153-156.
Vorteil beim Lesen? Optom. Contact Lenses, 2, 135-142.
European Conference on Eye Movements.
