Exploring the lived experience of age-related macular degeneration and health care use in Germany
Purpose: Health care for people with age-related macular degeneration (AMD) and visual impairment/blindness is complicated as it includes both medical care and low vision care offered by various providers without established coordination. This qualitative analysis aims at exploring experiences of people with AMD in daily life and with their health care including their information and help needs.
Material and Methods: This analysis is part of the qualitative arm of a wider mixed methods research project. As a sampling strategy, we pursued the goal of maximum variation. We conducted narrative, semi-structured interviews with people diagnosed with AMD all over Germany. The interviews were thematically analysed.
Results: Twenty-nine interview partners were included in this analysis. Experiencing AMD in everyday life meant (i) the perception of visual changes, (ii) dealing with blindness perceived as stigma, and (iii) social consequences. Their health care experiences were shaped by their individual information needs, questioning their communication with their ophthalmologists, increased time required for medical examinations and a great logistical effort in order to access both medical as well as low vision care. Support services in the framework of low vison care were well appreciated by our interviewees.
Conclusion: People with AMD have individual information and help needs that must be addressed and acknowledged in health care.
Introduction
Due to demographic changes, visual impairment and blindness are increasing, particularly age-related macular degeneration (AMD) followed by glaucoma and diabetic retinopathy worldwide are of concern. In Germany, there are about 6,938,000 people living with early stages and about 480,000 people affected with late stages of AMD.1
AMD is a degenerative condition of the macula that is specialized in central, highest spatial resolution and color vision. AMD is divided into three stages: early, intermediate and late. Early AMD has little or no impact on visual function (asymptomatic) and intermediate AMD shows usually just few symptoms (oligosymptomatic). Initial symptoms include distorted vision or central visual loss often pictured as “immobile, centrally situated grey spots”.2 (p. 514) In the late stage, a distinction is made between atrophic (dry) AMD and neovascular (wet, exudative) AMD (nAMD). Dry AMD leads to gradual loss of vision. However, orienting vision remains even in late AMD. In contrast, people with nAMD often experience sudden vision loss that, if left untreated, exceeds the threshold of legal blindness within a few days or weeks.2 NAMD has been able to be treated with vascular endothelial growth factor (VEGF) inhibitors for about 15 years,3-5 that can maintain or improve vision in 80 % of nAMD patients.5 In between treatments with anti-VEGF injections, people with nAMD undergo regular controls, including retinal imaging with optical coherence tomography.6 In contrast, there are few treatment options for atrophic AMD. Only vitamin supplementation has been demonstrated to slow its progression, but the effect is small.7 Some new therapy approaches show promising results.8 Even those diagnosed with nAMD for which effective treatments exists, medical treatment with anti-VEGF therapy meant a physical, psychological and temporal burden. Our previous findings on AMD experience found that the experience of injections is a dominant experience of the disease overall. The injection process induced varying levels of anxieties. Participants with significant vision loss wanted to discontinue therapy because they experienced the injections as uncomfortable without experiencing any positive effects. The doctor-patient relationship played a significant role in the emotional and physical experiences of the study participants.9 Our recent meta-synthesis on experiences of people with AMD showed the profound effect AMD has on the everyday lives of older people.10 Simple daily activities become challenging tasks in a population in which keeping independence is crucial. The loss of independence often led to a loss of self-esteem and self-worth, including feelings of sadness and frustration.10
In Germany there is no established rehabilitation programme for people with AMD and / or visual impairment until today. Health care for people with visual impairments and blindness is complicated as it includes both medical and low vision care offered by various providers without established coordination. In brief, low vision care for people with AMD includes both rehabilitative and support services such as training in orientation and mobility, socio-legal counselling and low vision counselling.11,12 People with low vision have little knowledge and information about support services that might help to improve performing activities of daily living.10,13-15 In addition, the access to service provision seems to be more random and not needs-oriented among older people with visual impairment.13 Therefore, this qualitative analysis aims at exploring experiences of people with AMD in daily life as well as with their health care experiences including their information needs.
Materials and methods
Study Design
This qualitative analysis is part of the mixed-methods study “AMD- Care: Age-related macular degeneration and its effects from the perspective of people with AMD and providers” that examined the barriers to and difficulties in utilising available services (low vision care) for people with AMD.9 The quantitative arm of AMD-Care investigated the knowledge of providers (ophthalmologists and ophthalmic opticians) about support services via online surveys and the qualitative arm explored the illness experiences and coping strategies of people with AMD via interviews.
Ethics Statement
The study was approved by the Medical School Brandenburg Theodor Fontane (AZ: E-01-20180418).
Sample and Data collection
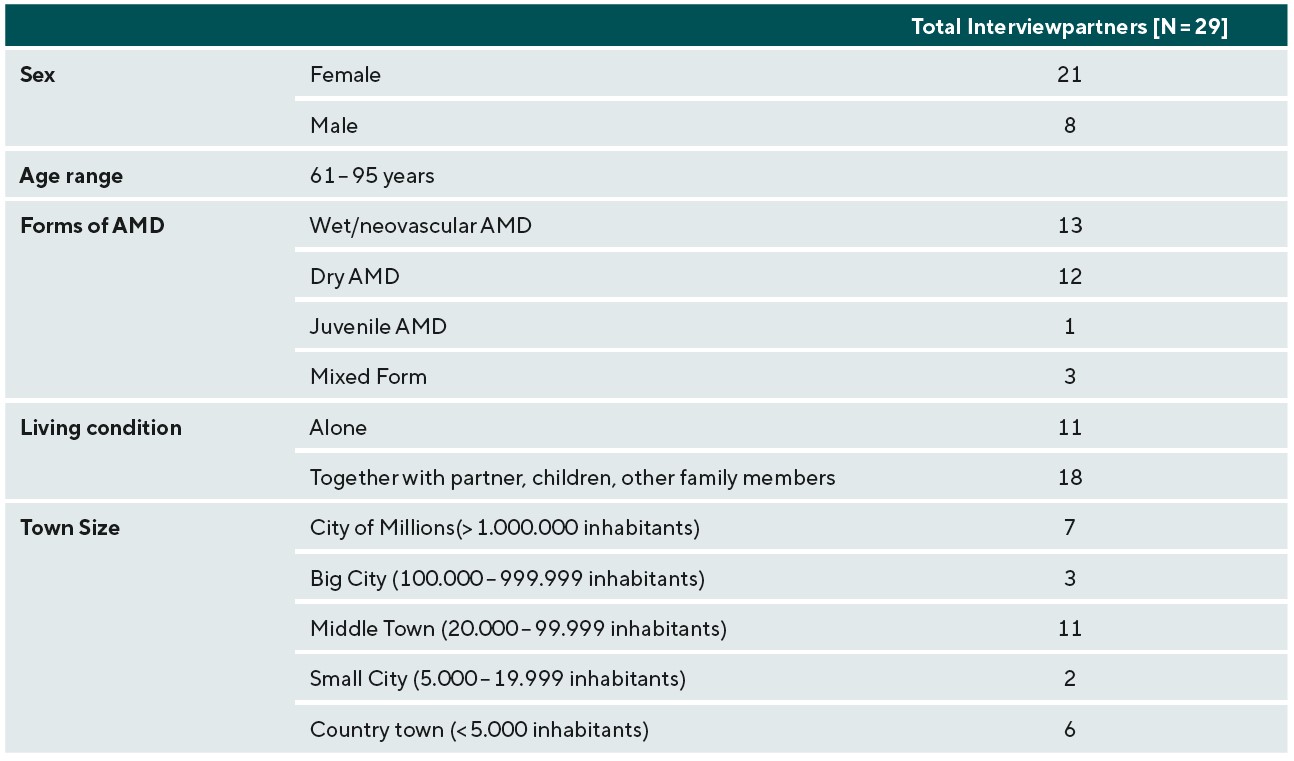
Sample selection for the overall study sample followed the research logic of grounded theory,16 which required a theoretically-based, successive selection of study participants in different disease-related, socioeconomic, cultural, and regional settings.17 As a sampling strategy, we have pursued the goal of maximum variation.17 Selection criteria for interview partners included: geographical aspects (e. g urban and rural areas, different regions from Germany), (ii) social aspects (living conditions: at home or nursing homes, married etc.) and (iv) medical aspects (e. g. time since diagnosis, form of the AMD, severity of the disease/visual impairment).. We recruited participants diagnosed with AMD who were above the age of 60 all over Germany between June 2018 and December 2020. Data collection has already been described in detail in Thier et al.9
Data analysis
The interviews were transcribed using F4 software. For data management transcripts were imported into MAXQDA 2020. The first author was responsible for the analysis with support by the last author. For this analysis, we only included the study participants who still lived at home in order to have a homogenous sample to study. We conducted a thematic analysis.18 To do so, we read each paragraph of the transcripts and coded them according to the concepts and ideas found in each paragraph. Then initial codes were clustered into two descriptive themes: experiencing AMD in daily life and health care experiences. This process was conducted iteratively, moving back and forth in the data. To develop analytical themes, we then used the OSOP (one sheet of paper) method.19 In regular meetings with members of the advisory board of AMD- Care as well as in data meetings of our institute’s internal research workshop, the analysis was monitored and the analytical themes were deepened.
Results
Sample
A total of 29 interviewees (21 female, 8 male) with AMD were included in this analysis. Demographic data are shown in table 1.
Analytical themes
Experiencing AMD in daily life
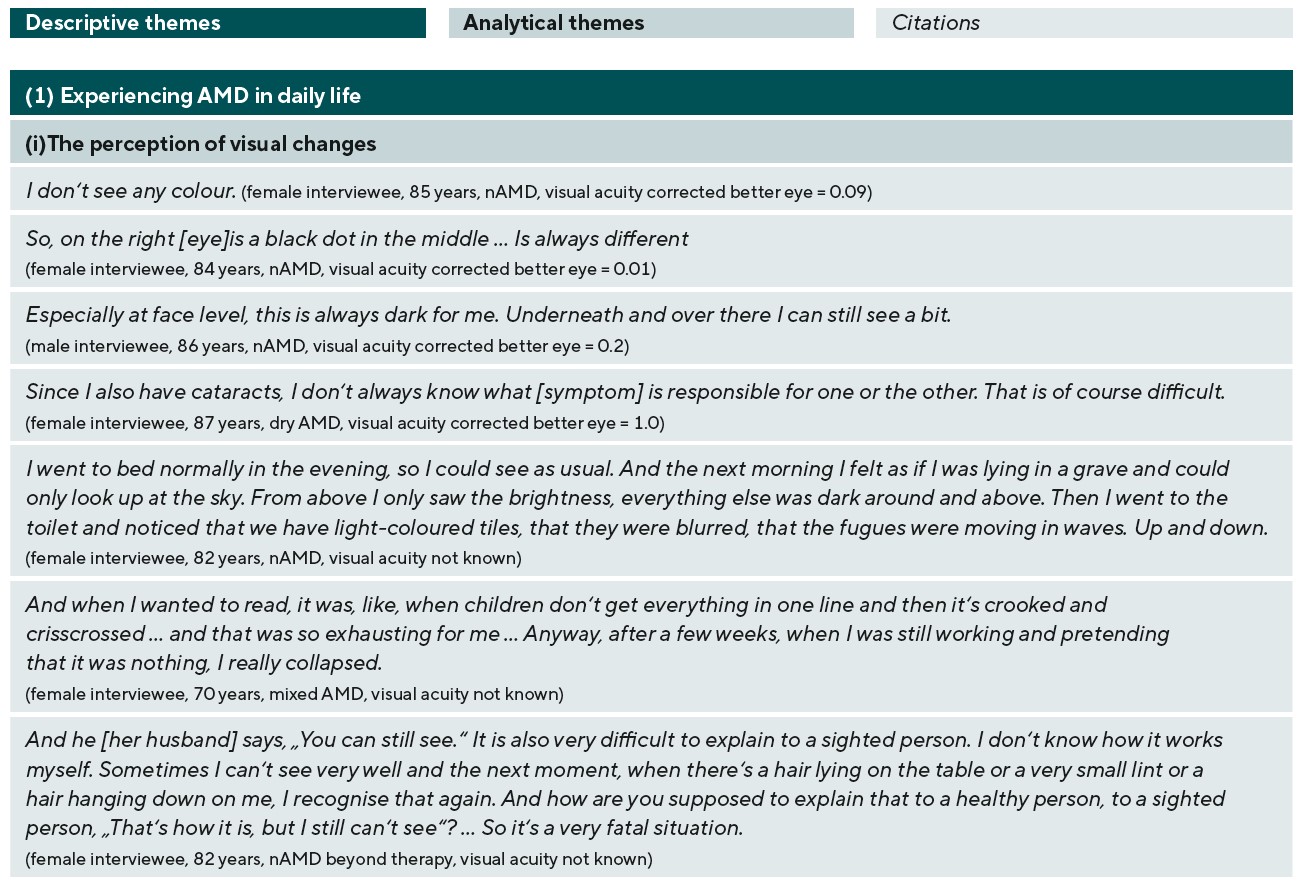
Experiencing AMD in daily life meant (i) the perception of visual changes, (ii) dealing with blindness perceived as stigma and (iii) social consequences. Corresponding citations for each analytical theme are presented in table 2.
(i) Perception of visual changes
The subjective visual impression of our interviewees differed individually. Almost all interviewees perceived visual changes or visual disturbances like distortions, blurred vision, loss of color vision, glare sensitivity and / or central dark spots varying in severity. Other diagnosed eye diseases, e. g. cataract and / or glaucoma, causing additional visual symptoms made it on the one hand difficult to know which disease was linked to which visual symptom and on the other hand made their visual experience more difficult. Only a few reported slight visual changes that were hardly noticeable in everyday life (table 2).
Many participants described that they perceived the visual disturbances suddenly and this made them feel worried and unsettled. The perception of visual symptoms was depicted as an enormous psychological burden by some participants in daily life. One interviewee explained that the distortions she experienced while reading were so bothersome that they resulted in a mental breakdown and the end of her self-employment as a psychotherapist (table 2).
Most of our interviewees characterized their vision as ever changing- between seeing and not seeing. Because of this, they reported experiencing conflicts in their social environment. One interviewee described that her visual perception caused difficulties in her social interaction with her husband as she could sometimes see things, even small things, and sometimes she could not see anything. In order to prevent social conflicts, our interviewees often tried to explain their visual experience to those closest to them, but that was often experienced as very difficult and frustrating.
(ii) Dealing with blindness perceived as stigma
As most of our interviewees imagined blindness as perceiving just “black” yet most were still able to see something, the distinction between visual impairment and blindness seemed of particular importance to them. Therefore, they emphasized that they were visually impaired but not blind. Blindness or becoming blind represented the greatest fear for all interviewees, as the interviewees often associated it with not being able to participate in life and found life less worth living. Occasionally, they related being blind with being unintelligent. One participant even implied that she would not want to live anymore when she became blind. Blindness was perceived as a stigma by many interviewees. They struggled or even rejected support services or aids associated with blindness, e. g. the white cane, the blind badge or contacting associations for the blind, as they were not able not identify with them and they felt stigmatized. However, some of our interviewees knew people who were blind in their social environment and this helped to ease the fear of becoming blind and overcome their prejudices. Such people became positive role models that the interviewees looked up to, from whom they learned that a life with blindness is still worth living and who gave an incentive to cope with life with a visual impairment (table 2).
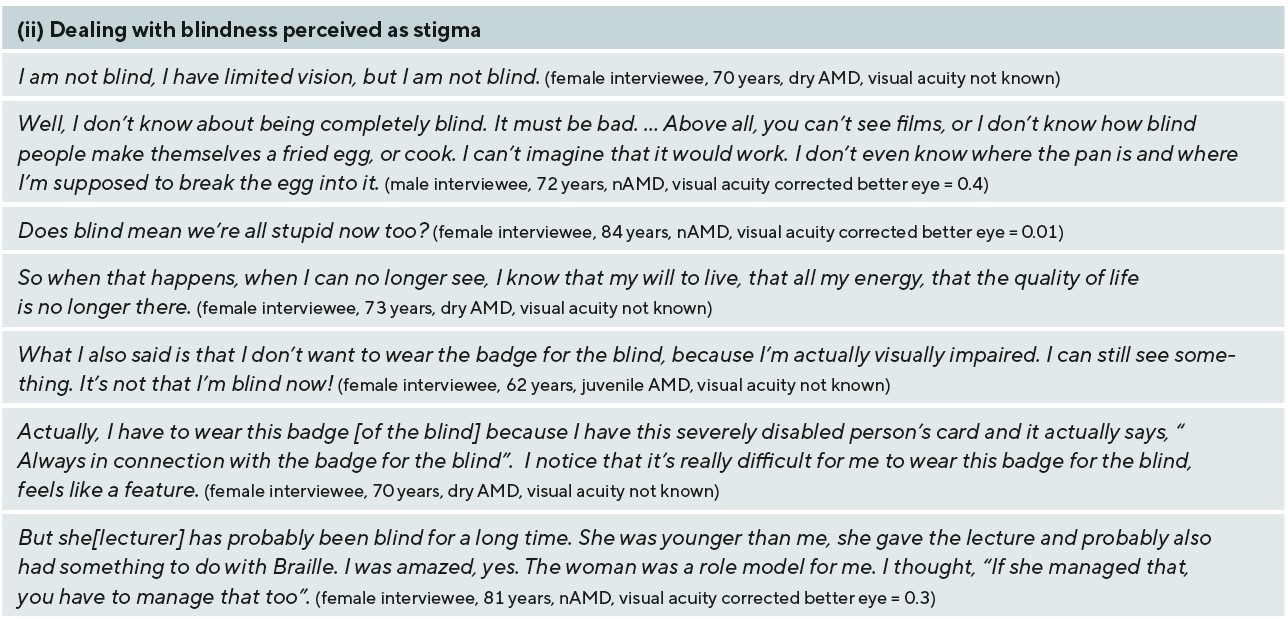
(iii) Social consequences
The majority of our interviewees described that their visual impairment had a significant impact on their lives and they mainly felt loss about the declined ability to read, drive and recognize faces. They explained that they tended to do very little in their daily lives and therefore missed highlights in their lives. Furthermore, they illustrated how they were suddenly no longer able to assess everyday situations due to the visual changes and thus lost control over them. As an example, they could no longer judge what was clean and dirty or how they were perceived by society. In some cases, this unsettled them so much that on the one hand, they were ashamed of their limitations and the associated effects and that on the other hand, they were constantly accompanied by fears in everyday life. One interviewee explained that she felt embarrassed eating in public as her difficulty eating with a fork and knife caused even her granddaughter making fun of her eating habits. In the course of the disease, our interviewees became increasingly dependent on the help of other people in their social environment. Many said that they initially struggled with taking on the role of the person in need of help or felt useless and / or ashamed asking and accepting help. Some interviewees said that relying on „help of strangers“ was difficult for them as they lacked confidence / trust in strangers.
However, most of the interviewees described that they got used to their visual impairment over time and learned to live with it in everyday life. The duration of time it took for the interviewees to adjust to living with visual impairment varied. Factors such as the acceptance of the visual impairment in the closest social environment, the use of aids and support services, embracing their new social role, the course of the disease and the personal attitude towards living with a disease played an important role. Interviewees who had a social environment that accepted their visual impairment and supported them found it easier to adapt, as they were better able to cope with activities of daily living. Those who lived with spouses or partners relied almost entirely on them. As mentioned above, some interviewees had difficulties accepting their new role as a person in need of help, especially if they had previously mainly taken care of their families and were no longer able to do so. The sooner they embraced this new role, the sooner they arranged to a life with visual impairment. With aids, e. g. magnifying vision aids, interviewees were able to maintain a certain degree of independence in daily life and thus found it easier to come to terms with the new situation. The interviewees whose AMD and visual impairment progressed gradually were able to adapt bit by bit. The majority of interviewees experienced additional health impairments, e. g. cancer, which they perceived as worse or even life threatening, making the visual impairment seem less severe and more acceptable. Some also mentioned that advancing age is often accompanied by age-related impairments that they have learned to accept.
Health care experiences
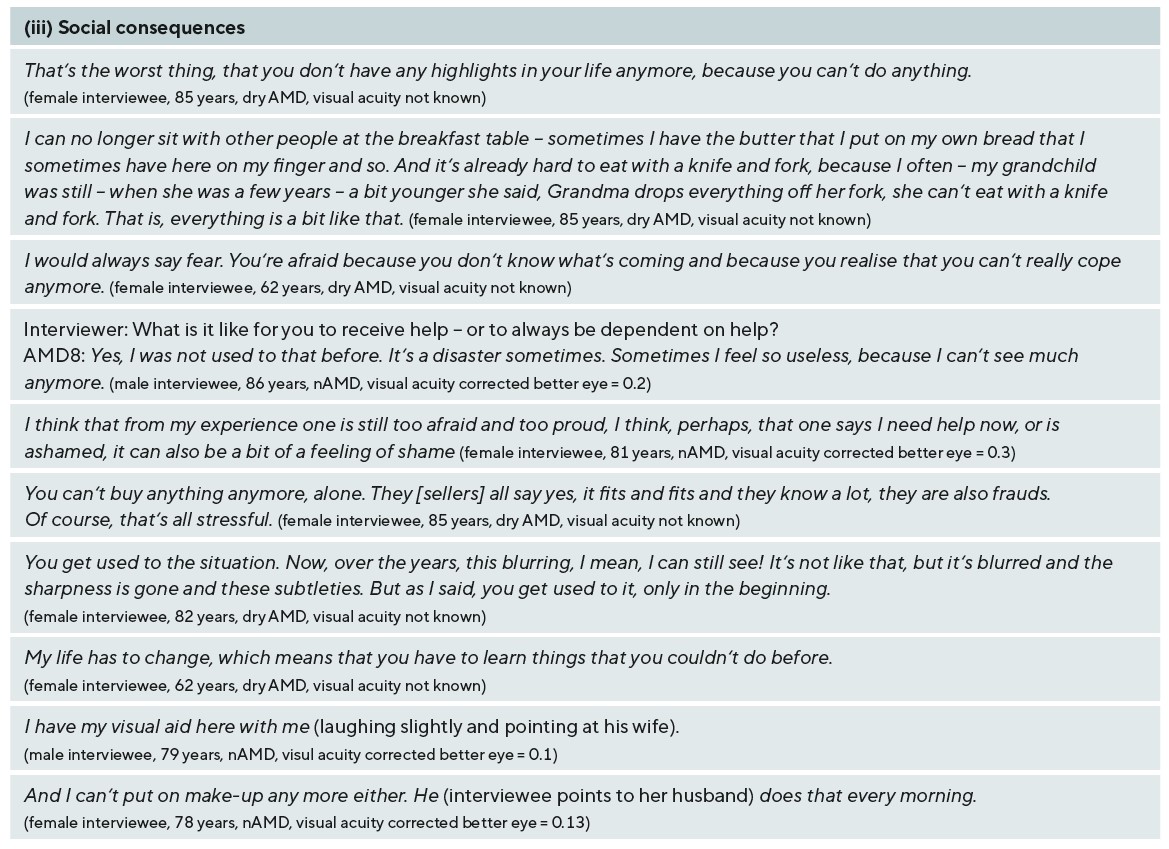
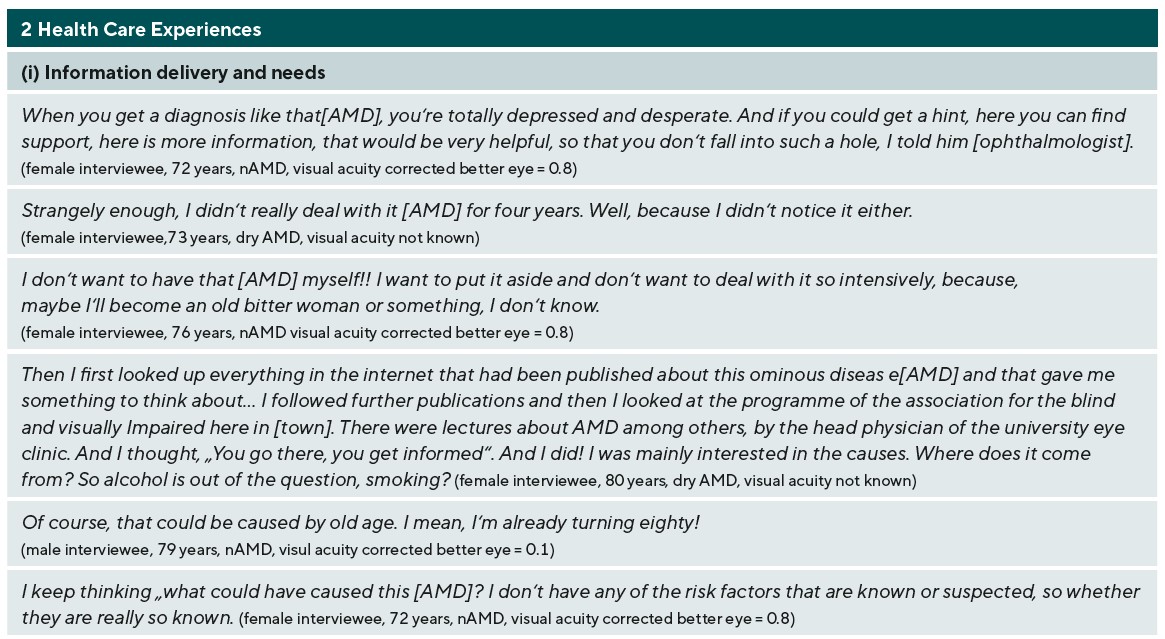
Our interview partners talked about their experiences with medical care as well with the provision with support services and aids (low vision care). In the analysis, four analytical themes emerged: (i) Information delivery and needs, (ii) talking with doctors, (iii) time consuming care and (iv) feeling understood by support services (table 3).
(i) Information delivery and needs
The majority of our interviewees illustrated the experience of being diagnosed with AMD as a „shock“. They explained that they have never heard about AMD at the point of diagnosis and the majority did receive just little information about the disease itself and support services from their ophthalmologists. Especially in the moment of diagnosis, our interviewees expressed the wish for more information about the AMD or support services. Some interviewees explained how information about support services might have been helpful for them to ease the psychological burden of the diagnosis. Throughout the interviews, our interviewees described very different individual information and help needs. These varied and seemed to be mainly influenced by the respective degree of visual impairment or the AMD, their general health condition, the coping phase they were in at the time, the social support and / or age.
Interviewees, who did not experience any visual limitations in their everyday life due to the AMD (respective degree of visual impairment or AMD), indicated that they did not feel the need to contend with the AMD and / or use possible aids or support services. Therefore, they narrated no need for more information or support in daily life. One interviewee who was very depressed due to sudden rapid progression of visual impairment said he had to first „come to terms with himself” and AMD before being receptive for further information or support (due to being in the coping phase). Another interviewee explained that she did not want to talk or hear more about the disease. She preferred to avoid confrontation with the disease. Some interviewees expressed no further need for support as they received sufficient support for completing daily activities by their immediate social circle (social support). As an example, one interviewee described that her husband started putting on her make up. The majority of the interviewees, especially those living alone, were very interested in and / or were in need for information about AMD and support services in the framework of low vision care in order to deal with the AMD and its effects in everyday life. Therefore, many interviewees informed themselves (with or without the help of their social environment) mainly via internet, print media and / or others diagnosed with AMD about the disease itself and support services (table 3). Beside information about support services, our interviewees were very interested in finding out what caused AMD. Some primarily blamed their increasing age. Others said they could not understand why they got AMD, because none of the known risk factors besides age applied to them.
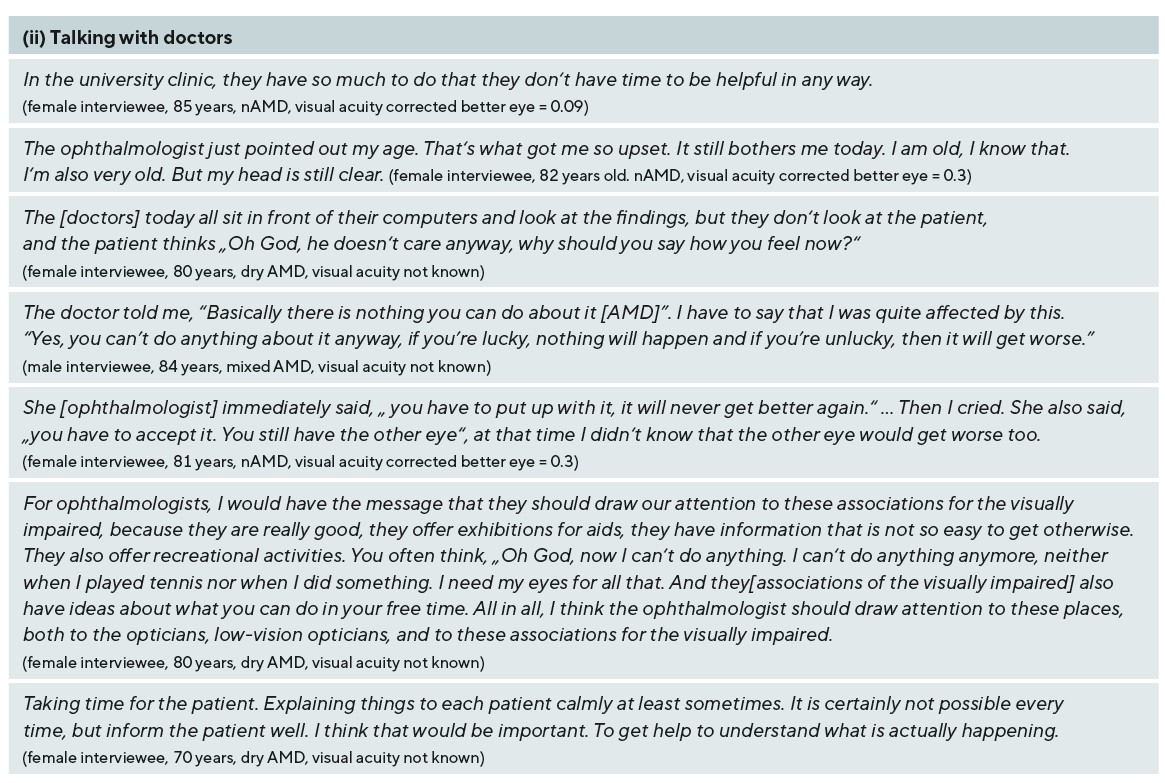
(ii) Talking with doctors
For the majority of our interviewees, their ophthalmologists were their central contact of care who they regularly consulted. While some of them felt well informed and cared for by their ophthalmologists, others felt they received insufficient information about the AMD and support services. Interview partners who detailed receiving insufficient information about AMD and support services from the ophthalmologists questioned their own ability to communicate with the ophthalmologist. Some interviewees admitted not asking enough (about the AMD in general and support services) and described being overwhelmed by the situation, not knowing what to ask, feeling not taken seriously and / or not wanting to burden the ophthalmologists’ workload with their problems. Some interviewees experienced that the ophthalmologists were not particularly attentive and therefore concluded that the doctors were not interested in their problems.
Occasionally, our interview partners felt that their doctors did not take them seriously because of their age. This was very frustrating and incomprehensible for them, as they felt that they were „still quite clear in the head“. Interviewees who were diagnosed with dry AMD or who could no longer be treated with anti-VEGF often heard from their ophthalmologists that „nothing more can be done“. This was shocking for them to hear and added to their stress. At the end of the interviews, our interviewees were given the opportunity to express messages to ophthalmologists. The interviewees mainly wished for more time and attention in their consultations and more education / information about support services.
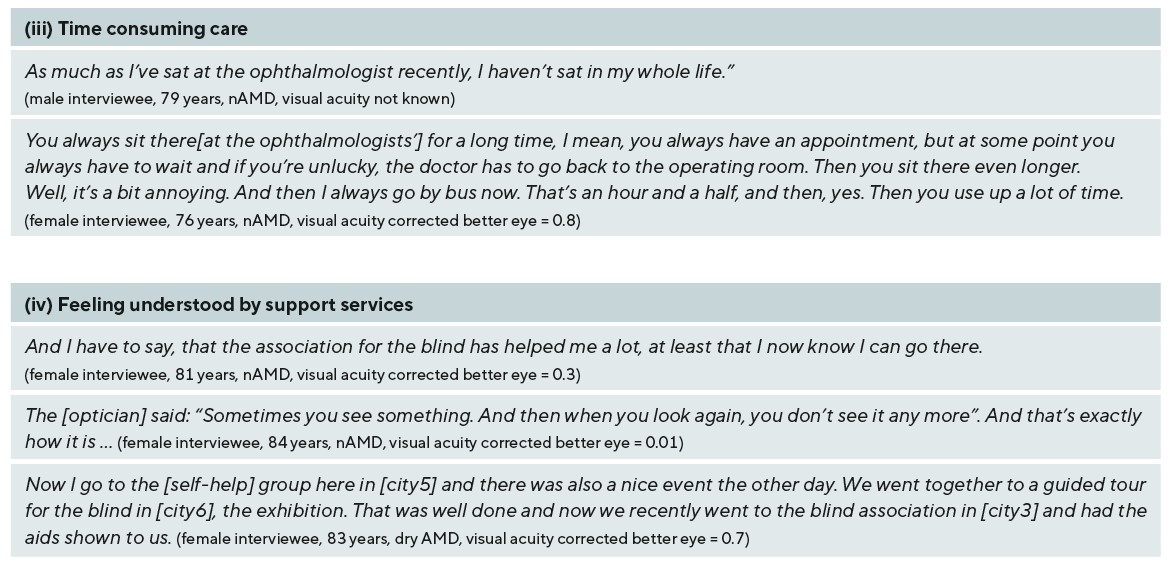
(iii) Time consuming care
During the regular visits to their ophthalmologists, our interviewees described how the respective facilities they visited were organized. A burden was described by the time required for treatments and examinations. Long durations were associated with the regular appointments, long waiting times and / or with travelling to the respective facilities. This was burdensome for many of the interviewees, especially for those who had other health conditions and they also described the difficulty and logistical effort needed to reach and access support services.
(iv) Feeling understood by support services
The majority of our interviewees used a variety of aids and support services (table 3) in order to adjust to a life with visual impairment. They described how the utilization of various support services, e. g. psychosocial counselling or further educational offers, or low vision aids, e. g. magnifying glasses, helped them in order to conduct daily activities, to find out more about AMD and / or to access other services that might be important for them. As part of these services, the interviewees experienced the opportunity to talk and exchange experiences with others diagnosed with AMD or other professionals in addition to medical personnel, e. g. social counsellors or ophthalmic opticians. Above all, they experienced understanding for their situation. Some regional associations of the visually impaired and blind offered special events that our participants appreciated very much, as they were “missing highlights in their life” before and so they could participate in cultural and social life again.
Discussion
The perception of visual disturbances was described by our interviewees as very stressful, as these restricted them in activities of daily living. The visual disturbances also led to conflicts with their closest social environment. Our findings indicate that their immediate family members, especially spouses / partners, represented a central point of care in order to deal with visual impairment in everyday life. Dyadic coping with chronic illness has been shown to be beneficial to both partners in numerous studies in that coping with the stress of illness together (we-stress) and a shared focus on the illness (we-disease) is positively related to each of the individuals. It also leads to better adjustment to life with the illness for both, higher relationship satisfaction and with more stable partnerships in the long term.20-24 Therefore, involving immediate family members in the education about AMD and low vision care services might help to increase the mutual understanding. Recognition of existing sight by the visually impaired person might help to alleviate social interaction between people diagnosed with AMD and their immediate family members.
The moment of diagnosis seemed to represent a major burden for our interviewees. The majority of our interviewees lacked information and expressed a need for information. The participants linked this to the inability to express their views to their ophthalmologists. The problem may lie with the fact that the information AMD patients need on support services, the ophthalmologists may not have. Casten et al. suggested that ophthalmologists do not inform their patients about low vision care as they are unaware of these offers themselves and / or they “fail to discuss them with their patients for other reasons”.25 (p. 3) Several studies investigating the information needs of patients in general found multiple reasons why patients do not receive satisfying information from their health care providers involving the following: under- or overestimating the individual information needs of patients, insecurity or reluctance of patients addressing their information needs and misunderstanding between patients and HCPs.26
Our findings showed that support services in the framework of low vision care were well appreciated by our interviewees. They used various support services: low vision and technical aids, further educational, psychological and social law counseling. In the literature, these support services are often referred to as low –vision rehabilitation services. However, evidence is still missing about the effectiveness of low- vision rehabilitation services.27,28 Low- vision rehabilitation is complex as it needs to be tailored individually on the one hand and on the other hand it involves a mixture of different kinds of interventions. As a result, studies examining the effectiveness of low-vision rehabilitation encompass a range of different interventions, comparisons, and outcomes. This makes it difficult to analyze or predict which kind of rehabilitative strategy is the most effective for supporting people with AMD. Similar types of rehabilitative and outcome measures within study designs might help to improve evidence-based research syntheses.27 Furthermore, in order to acknowledge the individual information and help needs of people with AMD a participatory approach to the development of a rehabilitative intervention strategy, the study design and the outcomes might alleviate existing challenges in the field of low-vision rehabilitation service research.27,28 The sample size is small, but this is not uncommon for qualitative research of this type. However, it may be that our study sample consisted of particularly active patients who were able to cope better than those not in this study. Those people with AMD who are less active may have different information needs than our sample expressed.
Conclusion
Our findings show how people diagnosed with AMD benefit from a supportive environment and low vision care in order to deal with visual impairment in everyday life. In addition, we found that people with AMD have individual information and help needs that should be recognized and addressed in their health care.
Conflict of interest
The authors have no conflict of interest on the methods and devices mentioned in the article.
