Globe Trauma, Aniridia and Prosthetic Contact Lens
Purpose. This case report describes the visual and cosmetic rehabilitation of a 63-year-old patient with a rigid prosthetic contact lens following penetrating globe injury, aniridia and traumatic aphakia.
Material and Methods. Based on corneal topography a rigid prosthetic contact lens was fitted to achieve both visual and cosmetic rehabilitation of the injured right eye. The Falco irisTruefit colour wheel from Falco lenses AG was used to determine the iris tint of the custom-made lens. The final refractive power of the lens was established by using a variable aperture pinhole.
Results. With the rigid prosthetic lens it was possible to achieve visual and cosmetic rehabilitation of the injured eye in accordance with the findings. Six weeks after the contact lens was fitted there was a significant improvement in visual acuity and excellent subjective and objective tolerance of the contact lens. The photophobia caused by the aniridia was significantly reduced. In addition, with the spectacle lens correction for the left eye, a positive stereopsis was achieved.
Conclusion. The visual and cosmetic rehabilitation of eye injuries with aniridia and traumatic aphakia has always been one of the classic indications for prosthetic lenses. For complex corneal shapes, treatment with mini-scleral prosthetic contact lenses should also be considered. The use of a variable pinhole has proven to be helpful in determining the contact lens power of the lens in the presence of aniridia and aphakia.
Introduction
Eye trauma is responsible for a large number of monocular visual impairments and blindness worldwide.1 In the USA, the estimated annual incidence of globe-opening eye injuries between 2014 and 2018 was 34,061. The overall prevalence was 1.58 cases per 100,000 per year. The average annual prevalence for men was higher at 2.28 cases per 100,000 people affected than for women at 0.89 cases per 100,000 per year.2 Bulbus-opening eye injuries are a severe form of ocular trauma, including tearing or rupture of the entire eye wall, and often require surgical treatment. They are associated with high morbidity.3,4 In a USA multicenter, retrospective, population-based cohort study, the authors identified a total of 740 injuries to the eye or adnexa in children and adolescents younger than 19 years over a period of 9 years. This corresponded to an incidence of 203 cases per 100,000 children. The mean age of the children was 10 years. Of these, 62.4% were male.5 The Birmingham Eye Trauma Terminology (BETT) system classifies globe-opening eye injuries as globe ruptures, penetrating eye injuries or intraocular foreign bodies or penetrating injuries.6 As a rule, a globe-opening eye injury requires primary closure of the cornea or sclera or surgical removal of the foreign body.7 Postoperatively, rigid gas permeable (RGP) contact lenses are often the treatment of choice for visual and cosmetic rehabilitation.8,9,10
Case description
A 63-year-old patient presented for the fitting of an iris contact lens for the right eye. The reason was an accident in 2017 resulting in a severe penetrating globe injury and aphakia as well as subsequent uveitis and associated vitrectomy. From 2017 to 2024, the patient underwent regular ophthalmologic care due to the uveitis and the complications associated with this condition. A secondary IOL implantation with an artificial iris implant, which was considered during this time, was not performed and instead the fitting of an iris contact lens was suggested. Cataract surgery on the left eye had not yet been performed despite relatively low visual acuity due to the posterior synechiae caused by uveitis. Due to the patient‘s enormous suffering in view of the high photophobia and low visual acuity in the affected eye and the resulting binocular vision impairment, the patient was extremely motivated for optical and cosmetic rehabilitation by treatment with an iris contact lens.
The most recent ophthalmologic diagnosis was as follows: Right eye status: post penetrating globe injury, traumatic aphakia, post anterior vitrectomy and left eye status: advanced cataract, posterior synechiae. OU: uveitis. Uncorrected visual acuity right eye: hand movement, left eye: 20/60p.
Material and methods
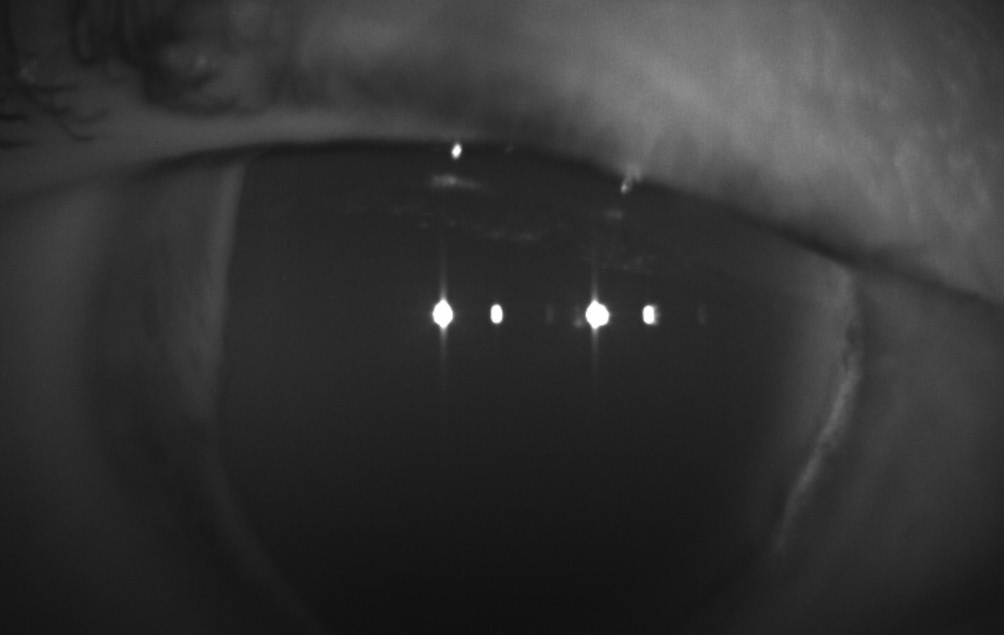
Apart from Aniridia no additional abnormalities in the anterior segment if the right eye were detected at the initial examination in our practice (Figure 1). The left eye showed an advanced cataract; the cornea was smooth and clear; posterior synechiae as a result of uveitis were visible. The eyelids and conjunctiva were free of irritation on both eyes. The tear meniscus was > 0.2 mm in the right and left eye; the tear film was normal. The corneal diameter in the left eye was 11.6 mm.
Refraction, visual acuity (and corneal topography of the right eye) were as follows:
Refraction (BVD 11 mm)
O.D.: +15.00 D cyl −2.25 D axis 166°
O.S.: −2.50 D
Visual acuity
O.D.: 20/200
O.S.: 20/50
Corneal topography OD
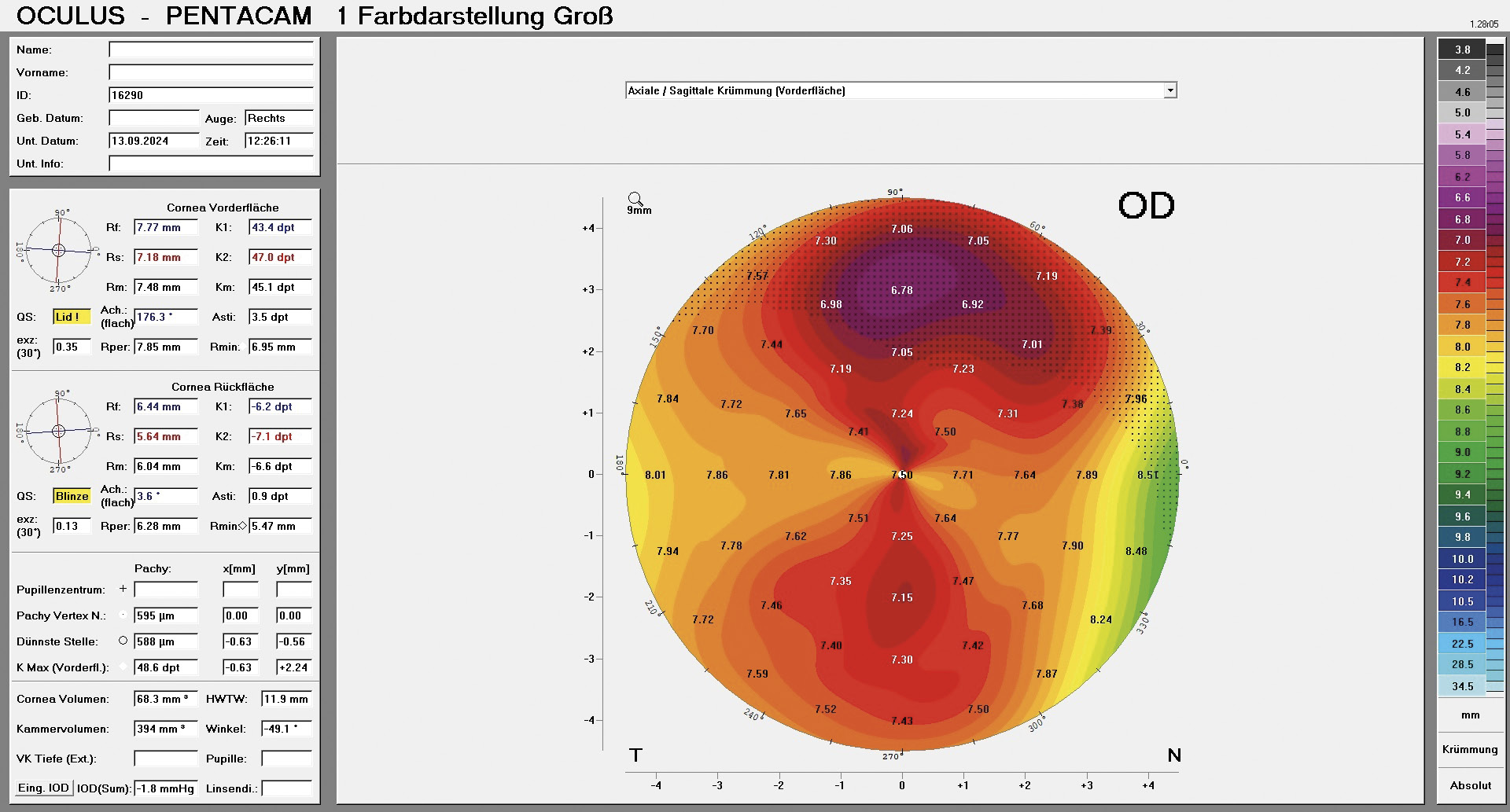
The central corneal radii by Oculus Pentacam (Oculus Optikgeräte GmbH, Wetzlar, Germany) were 7.77 mm at 176° and 7.18 mm at 86° with an average eccentricity of 0.35 (Figure 2).
Determination of lens parameters
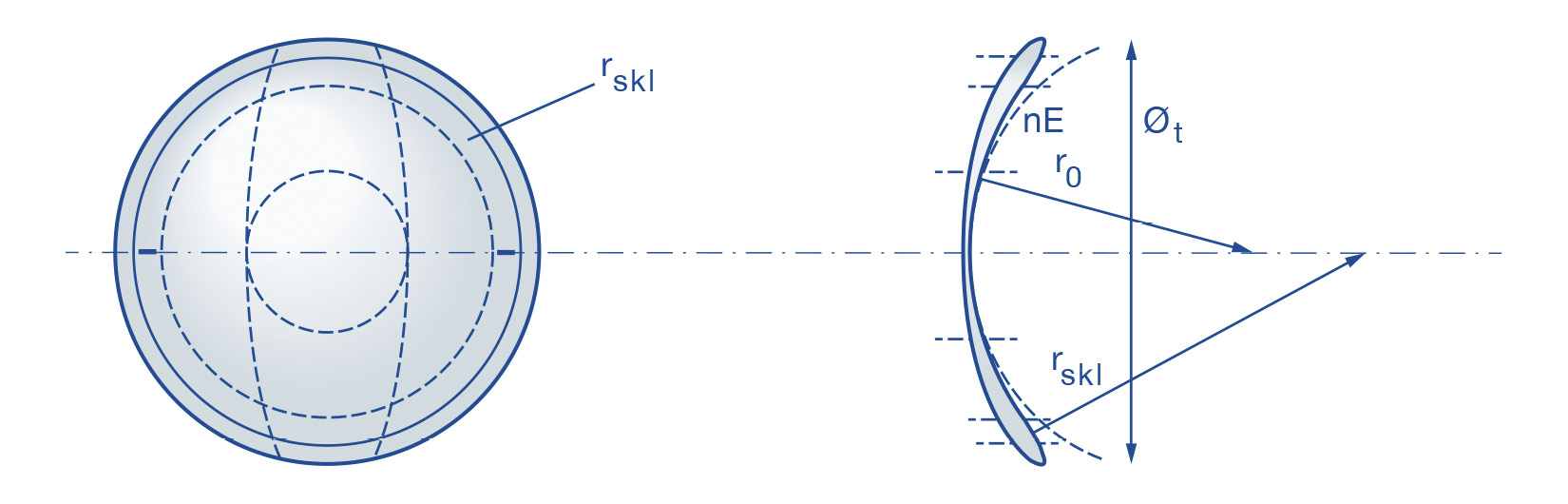
Based on the refraction, the corneal topography and the corneoscleral profile, we decided to fit a rigid aspheric, peripheral toric mini-scleral contact lens from Falco (Falco Linsen AG, Switzerland). The scleral zone radius and the diameter of the scleral zone can be individually selected for this type of lens in addition to other lens parameters (Figure 3). The parameters of the first diagnostic lens were as follows:
Diagnostic lens
Lens type: Falco SKAX
Base curve: 7.75 mm
Numerical eccentricity: 0.4
Overall diameter: 13.50 mm
Refractive power: +23.12 D
Scleral zone radius: 10.00 mm
Scleral zone diameter: 10.50 mm
Material: Optimum – Extreme white
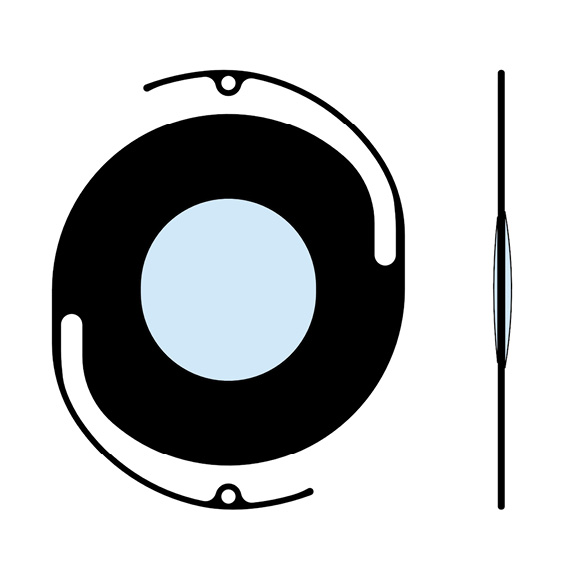
Both the central and periheral fit of the contact lens were excellent; visual acuity with contact lens (refractive power 23.00 D) was 20/100p. The final power of the iris contact lens was determined using a variable aperture pinhole (Bilosa, Austria) for a pupil diameter of 4 mm (Figure 4). The overrefraction was −2.75 D; the visual acuity was 20/80. The definition for the colour print was determined with the Falco “irisTruefit colour wheel”, which allows a good colour and structure determination of the colour print (Figure 5). The parameters of the prescription lens were as follows:
Prescription lens
Lens type: Falco SKAX
Central radius: 7.75 mm
Numerical eccentricity: 0.4
Overall diameter: 13.50 mm
Refractive power: +20.37 D
Scleral zone radius: 10.00 mm
Scleral zone diameter: 10.50 mm
Material: Optimum – Extreme white
The visual acuity with the prescription lens (O.D. 20/80), and the cosmetic effect of the iris contact lens were subjectively and objectively satisfactory (Figures 6,7,8). As the patient also required a vision correction due to the visual defect in the left eye (OS: −2.5 D), bifocals with the following correction data to achieve more stable binocular vision were prescribed:
O.D.: plano
O.S.: −2.50 D
Near addition: +2.50 D
This immediately resulted in simultaneous vision with stereopsis in the near distance.
Contact lens hygiene
Oté Clean was prescribed as cleaning solution, blink TotalCare as the storage solution and Concare saline solution as the rinsing solution.
Follow-up check: (5 weeks after lens delivery)
The following results were recorded:
O.D.: visual acuity 20/80
O.S.: visual acuity 20/50 (with spectacle correction)
Binocular: Stereopsis positive (near)
The patient was fully satisfied with the visual and the cosmetic rehabilitation. The visual acuity was satisfactory and the all-day tolerance of the contact lens was good. Photophobia was significantly reduced.





Discussion
Due to their complexity, open globe eye injuries are a challenge for patients, eye surgeons and optometrists. In this context, Andreoli M. and Andreoli C. published interesting data on the surgical rehabilitation of patients with open eye injuries. They analyzed the results of 848 injuries with 1415 surgical interventions. On average, patients had to undergo 1.7 surgeries and 7.1 follow-up examinations. Factors that required follow-up surgery included higher ocular trauma score, worse visual acuity before surgery, retinal hemorrhage, anterior vitrectomy at primary repair, pars plana vitrectomy at primary repair and lensectomy at primary repair.11 Rahman et al. analyzed records of 115 patients who underwent surgery at Manchester Royal Eye Hospital for open globe injuries. In 66 % of cases, the eye was injured with a sharp object, in 28 % of cases by blunt trauma. In 6 % of cases, the cause of the injury was unknown. The percentage of secondary enucleation in 107 open globe injuries was 12 %. Significant risk factors at first visit associated with eventual enucleation were relative afferent pupillary defect (P < 0.001), absence of fundus red reflex (P < 0.001), presence of eyelid injury (P < 0.02), blunt mechanism of injury (P < 0.02), and initial visual acuity less than 0.1 (P = 0.03).12 In many cases, aniridia is the result of eye injuries, but can also be congenital.13 Patients with congenital aniridia often have reduced visual acuity, dry eye, keratopathy and a number of other ocular and/or systemic conditions.14 Possible treatment options to reduce photophobia and improve visual acuity in acquired or congenital aniridia include soft or rigid iris contact lenses, an iris implant or corneal tattoos.15,16,17,18 In the presence of simultaneous aphakia, either implantation of an aniridia intraocular lens (IOL) (Figure 9) or fitting of an iris contact lens is possible.19,20,21,22 Fixation of the aniridia IOLs is either intracapsular or extracapsular.23 In the present case, a rigid iris contact lens was the method of choice for visual and cosmetic rehabilitation due to the complex ocular findings. The reason for a rigid (RGP) prosthetic mini-scleral lens was to achieve a stable fit of the contact lens with a high correction power and sufficient oxygen supply to the cornea. This avoids a possible vertical prismatic effect in a one-sided contact lens treatment and also ensures a stable cosmetic fit of the contact lens. A variable aperture pinhole is a great help for the final determination of the lens power in the case of high refractive errors and the presence of aniridia.
Conclusion
Fitting iris contact lenses is a safe treatment option after a globe-opening eye injury. In many cases this achieves a satisfactory monocular and binocular visual acuity, significantly reduced photophobia and improved cosmetic appearance, especially in the presence of aniridia and aphakia
Feng, P. W., Armstrong, G. W. (2021). Epidemiology of United States Inpatient Open Globe Injuries from 2009-2015. Ophthalmic Epidemiol., 28, 469-478.
Hammer, T. (2004). Kontaktlinsenversorgung als Möglichkeit der visuellen Rehabilitation bei Patienten nach offenen Augenverletzungen [Contact lens fitting as a possibility for visual rehabilitation in patients after open globe injuries]. Klin. Monbl. Augenheilkd., 221, 652-657.
Marty, A. S., Rabilloud, M., Fleury, J., Burillon, C. (2017). Prise en charge de l’aphakie et de l’aniridie post-traumatiques. Étude rétrospective de 17 patients opérés d’implants intraoculaires suturés à la sclère à iris artificiel. Gestion de l’aphakie-aniridie par implants suturés à la sclère à iris artificiel [Management of post-traumatic aphakia and aniridia: Retrospective study of 17 patients undergoing scleral-sutured artificial iris intraocular lens implantation. Management of aphakia-aniridia with scleral-sutured artificial iris intraocular lenses]. J. Fr. Ophtalmol., 40, 592-605
