Literature review and evaluation of the methods relating to the surface friction of soft contact lenses
Purpose. Numerous reports have hypothesised that there is a strong correlation between the contact lens (CL) comfort and its on-eye friction. Hence many methods had been developed, to measure coefficients of friction (CoF) of soft CL. The aim of this work is the review, evaluation and discussion of these methods.
Material and Methods. From the relevant literature, 15 methods published between 1995 and 2021 have been chosen based on their frequency of citation or because of their new or unusual approach. The evaluation focuses on the requirement that the method should closely mimic the CL on-eye situation. Moreover, it has been examined if these methods produce comparable results.
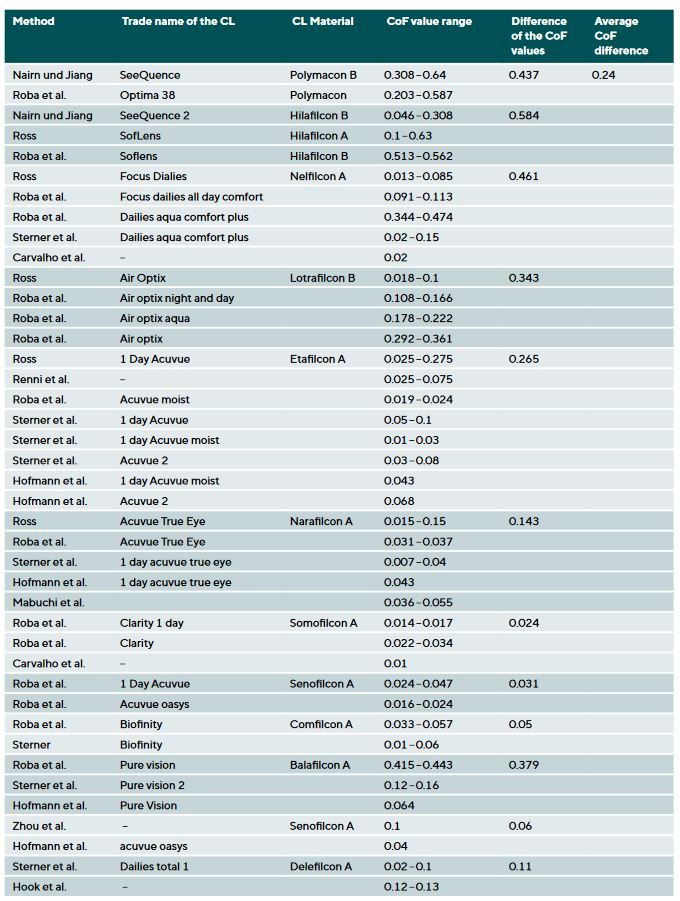
Results. None of the methods meet the requirements in every aspect and many show large differences in the used techniques. That includes the often used tribometer, a rheometer, a pendulum, an inclined glass plate and fingers. Moreover, it has been shown that the methods create a wide range of CoFs. For example, the material nelfilcon A, measured by five different methods, show values between 0.013 and 0.474. That is a difference of 0.461. On the other side, for narafilcon A the difference between CoFs is only 0.143.
Conclusion. To ensure that results from CoF measurements are valid and comparable between and within studies, a standardised method needs to be defined or developed. Choosing methods and parameters that simulate on-eye conditions would be beneficial in predicting wearing comfort and the effect of lubricating eyedrops. Thus, a more suitable method must be developed in the future.
Introduction
In Germany, around five million people wear contact lenses. 93 % of them being soft contact lens (CL) wearers.1 It has been observed that these figures have stagnated in recent years, both in Germany as worldwide. One of the main problems is a dropout rate of 10 – 50 % in the first three years of CL wear.2 Dropout is defined here as the proportion of CL wearers who have given up wearing CL. Contact lens discomfort (CLD) was cited as the most common reason to stop wearing contact lenses.3 The problem with CLD is that it cannot be measured objectively. It is an individual perception and can therefore only be determined in subjective surveys. As there is also an economic interest in retaining CL wearers as patients, methods had to be found to record or predict CL comfort with the aim of optimising both CL and care products in terms of short and long-term comfort. This would make it possible to assess the tolerability and comfort of new CL materials and care products as well as wetting agents before they are launched on the market.
The current literature considers friction between the CL and the upper eyelid during blinking to be a decisive comfort factor in addition to others.4 Kern et al. found that the subjective comfort on a scale of one to ten drops by one scale point as soon as the friction increases by a value of 0.25.5 This was also confirmed in another study.6 It is also assumed that increased friction due to reduced lubrication can lead to dry-eye symptoms, such as burning and itchiness.7 The risk of lid wiper epitheliopathy also increases.8 Friction between the upper eyelid and the anterior surface of the CL is, therefore, considered more critical than friction between the posterior surface of the CL and the cornea.7 It has also been found that increased friction is associated with an increase in cell damage.9 As there is currently no standardised measurement method for this important factor, the statements on this regard should be critically discussed. When developing the measurement method, most studies claim that the data measured in-vitro corresponds to the data measured in-vivo. The physiological conditions that affect the CL during wear are modelled in the measurement setup or measurement protocol. The variable measured is the coefficient of friction (CoF). The CoF is not a material constant and must always be linked to the measured system. It is a unitless quantity of friction and is calculated by dividing the applied normal force FN by the frictional force FR.
The aim of this work is to present the methods that have been used to date to measure the dynamic surface friction of soft CL. These were then evaluated and discussed.
Material and methods
The methods considered in this study were selected based on how frequently they were cited in the literature or because they pursue new or unusual approaches. Each component of these methods relating to friction is discussed and evaluated regarding how well they apply to the CL-on-eye situation.
The measurement methods should mimic the physiological conditions of the eye. Thus, an overview of the conditions should be considered beforehand to be able to assess the requirements of the CoF measurement methods. The behaviour of the CL on the eye should also be considered.
A well-fitted soft CL centres itself on the cornea and adapts to its shape. It covers the limbus by 1 – 2 mm and rests on the conjunctiva. It does not sit directly on the cornea or conjunctiva, but “floats” on the tear film (TF). There is also a thin layer of TF on the front of the CL, which ensures that the upper eyelid can glide over it with as little friction as possible when blinking.
During CL wear, the lens moves slightly and is rewetted every time we blink. The blinking frequency is normally between 12 and 15 blinks per minute. When blinking, the eyelid moves mainly vertically downwards and to a small extent horizontally in the nasal direction.10 The speed of the downward movement (closing the eye) is approximately 20 cm/s.11 Other sources assume a speed of 15 cm/s.7 The speed when opening the eye, on the other hand, is only half as fast at 10 cm/s. The eye is closed for about 30 milliseconds between movements, and the total blinking time is between 250 and 300 milliseconds. While blinking, the CL experiences a nasal upward movement. This is induced by both the upper eyelid and the lower eyelid, which moves horizontally in the nasal direction.11 It should be noted here that it is not the entire inner side of the upper eyelid that rests on the CL and rubs against it, as is the case with the lower eyelid, but that it is only the edge of the eyelid or the lid wiper. The lid wiper is part of the conjunctiva and is responsible for distributing the preocular TF over the eye.12 The length of the gliding movement of the upper eyelid is primarily determined by the size of the palpebral fissure. This varies from person to person, but is normally in the range of 7 – 10 mm for men and 8 – 12 mm for women.13 When blinking, a variable amount of pressure is exerted on the eye. For example, if blinking is triggered by glare, the pressure is approximately 3 mmHg. If the eyes are squinted more tightly, on the other hand, a pressure of up to 50 mmHg can be exerted.11 This pressure has also been investigated in various studies and shows relatively widely differing results ranging from 8.0 ± 3.4 mmHg 14 to 16.25 ± 6.18 mmHg in healthy eyes and 20.23 ± 5.73 mmHg in dry eyes 15 up to values between 0.2 and 0.25 N.7
In addition to the friction between the upper eyelid and the anterior surface of the CL, there is also friction between the posterior surface and the cornea. This means that the physiological conditions regarding this friction must also be clarified. The movement of the CL on the eye is induced both by eye movements and by blinking. The gliding distance is approximately ± 1 mm and the CL performs a rotating, nasal upward movement. During blinking, the CL is slightly pushed along with the eyelid movement. After blinking, it then slides down a little again.11 The speed of the CL is approx. 0.49 ± 0.21 mm/s according to a push-up test.16
Between two blinking instances, the CL is exposed to two temperatures. The first is the temperature of the corneal surface, which is approximately 34 – 35 °C.17 The anterior part of the CL however is exposed to the temperature of the surrounding area, the upper eyelid and the TF.
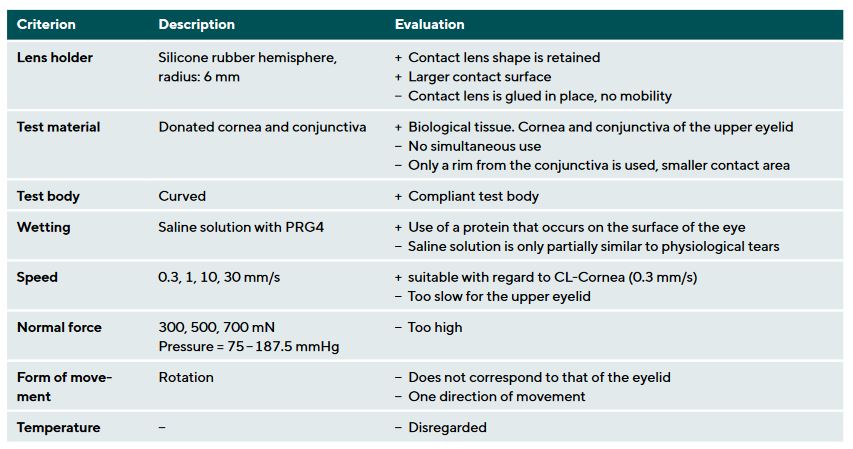
These physiological conditions established the criteria based on which the methods were evaluated and discussed. These criteria are the CL holder in the device, test material and shape of the surface against which the CL rubs, type of wetting, speed and direction of the friction-inducing movement, normal force or the pressure under which the friction occurs and temperature. Table 1 shows an example of how the criteria were evaluated. A “+” stands for a positive and a “−” for a negative evaluation.
Results
The methods analysed refer to the following studies: Nairn and Jiang (1995)18, Rennie et al. (2005)19, Dunn et al. (2008)20, Ross (2009)21, Roba et al. (2011)4, Zhou et al. (2011)22, Tucker et al. (2012)23, Koller (2014)24, Samsom (2015)25, Silva et al. (2015)26, Sterner et al. (2016)27, Hofmann et al. (2016)28, Hook et al. (2019)29, Carvalho et al. (2021)30 and Mabuchi et al. (2021)31.
A variety of different measurement conditions have been observed for the measurement of friction on soft CL.
The CL holder consisted of a flat surface made of plastic, a hemisphere made of plastic, silicone rubber or acrylic, a stainless-steel sphere, a convex surface made of polypropylene, a plastic hemisphere with Teflon housing, a device made of aluminium, a liquid chamber with a metal holder or no holder at all or a finger were used.
The test material ranged from plastics such as polymethyl methacrylate (PMMA), polyhydroxyethyl methacrylate (PHEMA), polyethylene terephthalate (PET), polyurethane (PU), borosilicate and glass discs with various coatings to stainless steel, Teflon, artificial and donated corneas and the skin of a finger.
The shape of the friction-inducing surface was a flat disc, a sphere of various sizes, a wheel, a curved surface or a ring.
Commercially available rewetting agents, saline solution, blister solution, a culture medium for artificial corneas, a liquid that mimics the composition of the TF (Tear-Mimicking-Solution=TMS), water or CL care products were used for wetting.
The speed of the movements ranged from 0.063 mm/s to 200 mm/s, whereby the direction of movement could be described as rotating or, as in most cases, linear as in a “back and forth” movement.
The normal force varied between 0.25 mN and 770 mN.
An overview of the CoF determined by the various methods can be found in Table 2. Some of the values are very high for the friction of a CL on the eye and should therefore be viewed with caution.
Discussion
All methods displayed different approaches.
The following section discusses which components are important for an ideal measurement setup and which of the methods considered came closest to this.
The CoF, which was determined in most methods, refers to a system comprising a base body and the material rubbing against it. It is not a material constant. There are two points at which the friction on the CL can be determined. Firstly, the friction between the edge of the upper eyelid and the anterior surface of the CL. Secondly, friction which occurs between the back of the CL and the cornea or bulbar conjunctiva. Most of the methods presented related to the upper eyelid-anterior surface of the CL system. However, some methods also referred to the posterior surface of the CL or made it possible to measure both the posterior and anterior surface of the CL.
In a measurement setup in which both the edge of the eyelid and the cornea are replicated and the CL is located in between, it is possible to measure the friction at both points simultaneously. The interaction of all these components allows to draw conclusions about the perception of comfort by the patient. However, if the goal is to optimise the posterior surface geometry of a CL in terms of friction, a measurement setup that does not take the anterior surface into account and only determines values that relate to the posterior surface would be more helpful.
A component of the measurement methods that was discussed in all studies was the normal force. One explanation for the varying normal forces is the different test bodies used and their resulting contact surfaces. As the pressure on the contact area results from the normal force, the normal force was adjusted in relation to the contact area. Therefore, even with an ideal test setup, the normal force should be determined considering which test surface is used. However, it should be questioned whether the value of the pressure generated by the entire upper eyelid should be used. This pressure would be appropriate for the friction measurement at the posterior surface of the CL, as the entire CL is exposed to the pressure there and rubs against the cornea. However, it should be noted that the CoF is independent of normal force and pressure and any changes in the measured values caused by these parameters indicate that the value measured is not only friction-dependent. When measuring the anterior surface of the CL, it should be noted that friction occurs primarily at the edge of the eyelid and that this may exert a different pressure on the CL than the entire eyelid. As the pressure of the upper eyelid varies from person to person, an average value should be established to compare the measured values.
Regarding the speed of movement, we should distinguish at both measuring points on the CL between the opening and closing of the eye. The speed of a well-fitted CL should be used as a benchmark value for the measurement at the posterior surface of the CL. This is approximately 0.491 mm/s.16 The problem with most of the methods studied is that the required speed was not achieved. In most cases, this is due to the limitations of the test equipment, as the combination of low normal forces with high speeds is difficult to obtain. It is therefore generally easier to measure the friction between the posterior surface of the CL and the cornea, as only lower speeds must be achieved here.
One point of criticism present in all methods except those of Mabuchi et al. and Koller is that only a small section of the CL surface could be measured.24,31 This was partly due to the fact that only a punched out or cut-out part of the CL was used, or that there was only a small contact area with the test body due to its shape. Ideally, the shape of the test body and the base body should create a conformal contact surface that allows measurement over the entire surface of the CL. This is necessary as otherwise the region of the bevelled edge is not included in the measurement results. Regarding the measurement at the anterior surface of the CL, an elongated contact surface would therefore make sense so that it corresponds to the shape of the lid edge. For the posterior surface measurement, the contact area should correspond to the entire posterior surface of the CL.
The CL holder should maintain the curved shape of the CL and many of the studies considered met this requirement. This was accomplished by using hemispheres on which the CL was placed or fixed. The hemisphere should correspond to the shape of the base curve of the CL. It is questionable whether a CL should be fixated in the measurement setup, as it is also not fixed on the eye and moves freely while blinking. If the CL were to be fixed for measurements at the anterior surface, this could result in higher CoF values as the CL cannot move. The material of the holder must also be taken into consideration depending on whether the CL is fixed or not. If the CL is fixed, the quality of the surface of the material is negligible as it hardly interacts with the lens. However, if the CL can move freely, the holder should have a surface that mimics the neighbouring tissue.
A variety of different materials and geometries were used as test bodies. Organic tissues such as donated corneas and eyelids or artificially grown epithelial tissue correspond to the conditions in the eye and should hence be used for the ideal measurement setup. It should be noted that the reproducibility of the results is limited since uniformity cannot be guaranteed. No clear statement can be made regarding the suitability of plastic, glass or stainless steel, as the similarity to eyelid and corneal tissue has not yet been tested. As already discussed, the shape should be based on the requirements for the contact surface. For test bodies that mimic the edge of the eyelid, this means that they must have an elongated, curved edge. If corneal tissue is used, this should have the shape of a hemisphere with the curvature of the base curve of the CL.
So far the type of movement and the associated glide path have been very limited in the available test methods due to the test devices used. The test devices used in the studies considered were only able to perform rotating or linear movements. These movements are too simple for the ideal measurement setup. Regarding the simulation of the movement of the eyelid or the edge of the eyelid, the movement would have to be primarily linear forwards and backwards, but also slightly lateral over a distance that corresponds to the width of the palpebral fissure. The movement of the CL on the cornea should be slightly rotating with a “back and forth” movement. These demands on the movement require a test device that can perform complex movement sequences. However, combining this with high speeds is difficult. For a feasible movement that still resembles the movements in the eye, a linear “back and forth” movement could therefore be considered suitable.
In order to match the in-vivo conditions in terms of wetting, it is easiest and most similar to the natural conditions to use artificial TF. However, it is important that it has the same properties as the real TF. Some of the studies discussed the viscosity of the wetting agent, observing that a higher viscosity leads to lower friction. This means that wetting agents to be developed in future should have a high viscosity with otherwise constant properties.18
None of the methods discussed here took the temperature of the eye into account, with the exception of the method according to Sterner et al.27 However, some studies did consider that the tests were to be performed at a constant room temperature.
Most of the measurements were carried out using micro- or nanotribometers, whereas the latest methods are based on pendulum technology. The ideal measuring device would have to allow for the required speeds, normal forces, motion sequences and the corresponding modifications for holding the CL to be achieved. It would also have to be sensitive enough to detect low CoF values. None of the methods could fulfil the combination of all these requirements.
The two methods that came closest to fulfilling this goal were those by Samsom et al. and by Mabuchi et al.25,31 Samsom et al. have a sound methodology regarding the use of eyelid or corneal tissue and the type of contact surfaces. Their measurement setup also makes it possible to measure the anterior and posterior surfaces of the CL independently as well as both at the same time. However, the form of movement, normal force and speed of this method could be improved. In addition, the method obtained high CoF values, which appear unrealistic, especially with regard to static friction.25 Mabuchi et al. used good contact surfaces and CL support, which would, however, have to be supplemented with organic tissue. In addition, their approach enables an almost desirable speed without having a contact surface that is too small or unsuitable.31
On average, the results of the measurement methods differ by 0.428 for the CoF. This emphasises that the methods do not provide the same values and are therefore not comparable. This demonstrates the need for a standardised measurement method.
Conclusion
The requirements for measurement methods that correspond to the conditions in the eye discussed in this paper are idealised. These requirements cannot necessarily be realised, as has already been partly noted. This is largely due to the limitations imposed by the measuring devices.
The methods considered here for evaluation and discussion were selected because they were frequently cited in studies regarding the friction caused by CL.
We could not make specific claims for some components of an ideal measurement method, since these are partly dependent on the CL used and other values the method is based on. This means, for example, that no statement can be made about the necessary normal force, as no clear average value is known for the pressure and the literature only mentions a range in which this pressure could lie.
It should be emphasised that there is no standardised friction measurement method that mimics the conditions in vivo. Values measured using existing methods cannot be compared with each other due to the different measurement conditions. Only data collected within one method are comparable and allow to compare different materials.
This paper provides an overview of the elements that should be considered when developing a measurement method while providing the basis for evaluating existing methodologies.
Conflict of interest
The authors have no conflict of interest with respect to the methods and devices mentioned in this article.
COE-Fortbildungsprüfung
The publication "Literature review and evaluation of the methods relating to the surface friction of soft contact lenses" has been approved as a COE continuing education article by the German Quality Association for Optometric Services (GOL). The deadline to answer the questions is 1. November 2025. Only one answer per question is correct. Successful completion requires answering four of the six questions.
You can take the continuing education exam while logged in.
Users who are not yet logged in can register for ocl-online free of charge here
Epitheliopathy. Prog. Retin. Eye Res., 53, 140–174.
Tran-Son-Tay, R. (2008). A Novel Method for Low Load Friction Testing on Living Cells. Biotechnol. Lett., 30, 801–806.
Tran-Son-Tay, R., Sawyer, W. G. (2008). Friction Coefficient Measurement of Hydrogel Materials on Living Epithelial Cells. Tribol. Lett., 30, 13–19.
Ophthalmol. Vis. Sci., 53, 6093.
Smulders, N., Gerhardt, L.-C., Valster, S. (2016). In-Vitro Method for Determining Corneal Tissue Friction and Damage Due to Contact Lens Sliding. Biotribology, 5, 23–30.
