Myopia Management Need in Germany
Purpose: The increasing prevalence of myopia, particularly in Southeast Asia, and the predicted increase of the prevalence of myopia in Western countries mean that more children will benefit from myopia management. The current study evaluated by retrospectively analyzing electronic health records from eye health care practices in Germany how many children receiving single vision correction showed an annual myopia progression that indicates the need of myopia management (MM).
Material and Methods: The Euronet database with a total data set of > 1 million orders from the years 2000 to 2020 served as the basis for the present analysis. The dataset was filtered by age (6 - 14 years), refractive errors and the presence of longitudinal order data (baseline and second visit after 11 - 24 months, n = 64,825). First, the database was filtered to only include children with a myopic refraction of the right eye (in
terms of the SE) of −0.5 D or below (n = 52,936). Next, the database was divided into children with an annual progression of the SE of ≤ −0.5 D (as a criterion for the need of MM, n = 25,432) and children with an annual progression of > −0.50 D (n = 27,504), respectively. The number of children that require MM per shop per year was evaluated and the groups were further characterized with regards to the distribution of baseline SE and SE progression.
Results: The analysis revealed that there are children of all ages who require myopia management, while their number increases with age, reaching a maximum at 10 to 11 years and declining afterwards (60 % of all children at age 7 and 30 % of all children at age 14, respectively). Children who have an early onset and high progression have baseline SE of around −1.50 D to −1.75 D and a second prescription SE of around −3.00 D. In contrast, children with later onset and lower progression have a similar baseline SE (average −1.62 D) but develop a second prescription SE of only around −2.00 D.
Conclusion: Awareness of myopia, its progression and its potential impact on eye health needs to be raised in Germany. Even though the absolute number of children requiring myopia management is still rather low compared to other regions, the baseline refraction of myopic children is already very high. It is important to note that children who require myopia management benefit from efficient treatment options.
Introduction
In recent decades, an increase in myopia has been observed, especially in South-East Asia, where the prevalence reaches levels of up to 90 %, and about 20 % of myopic children and adolescents show high myopia.1-3 Research on the internal and external causes for the increased prevalence, levels of and progression of myopia myopia shows that myopia is an adaptation of our visual system to our changing lifestyle, characterized by close distance reading and limited time outdoors, to only name a few key factors. As a results, not only is the prevalence increasing, but also the amount of myopia. The elongation of the eye is known to be the main driver of myopia and its progression. What is also known is that this elongation leads to ocular complications such as higher prevalent risks of glaucoma and chorioretinal abnormalities (retinal detachment, chorioretinal atrophy and lacquer cracks). In consequence, adults with high levels of myopia (< −6.00 D) are also more likely to have optic disc abnormalities (such tilted, rotated, and larger discs).4 Besides the potential negative influence on ocular health, poor or inadequate distance vision impacts on childrens’ quality of life and psychosocial functions.5 Social stigma and teasing have been widely reported in children wearing spectacle lenses,6 and reports have revealed that myopia might lead to lower self-esteem, especially in children with higher levels of
symptoms.7
Its potential impact on ocular health makes myopia one of the most important optometric and ophthalmologic health threats of the present and future. Behavioral, optical, and pharmacological methods are being intensively researched and tested worldwide to manage the onset and progression of myopia. This has led to a range of evidence-based interventions that can be integrated into routine practice. Accordingly, attention is rising on how myopia is treated around the world. Since 2015, Wolffsohn and co-authors systematically collect feedback from practitioners to analyze myopia management strategies applied in clinical practice, with the most recent update in 2022.8-10 Until 2019, eye care practitioners showed high concerns regarding the prevalence of myopia, but still most of them used single vision lenses for myopia correction. Only in 2022, the use of myopia management interventions increased significantly, although there were still differences between and within continents. As the management of myopia and its consequences require additional professional training, attitudes and sometimes new equipment, McCrann and co-authors posed this question: “Is optometry ready for myopia control”? Their analysis revealed that optometrists feel that they need more knowledge about the etiology of myopia and successful strategies of myopia
management.11
One important point has not been addressed yet and that is the number of individuals in the need of myopia management. The first question that arises here is to ask, when to qualify children in the need of management of myopia. A potential and often applied threshold used is the annual progression of the spherical equivalent refractive error. Using this, any progression ≤ −0.50 D is defined as being subject to the need of myopia management, while annual progressions > −0.50 D are classified as not in the need of myopia management. As there seems to be agreement between both researchers as well as clinicians on this threshold, it was applied in the current analysis. Nevertheless, it needs to be pointed out that also children with lower annual progression might benefit from myopia management. The current analysis presents results from such an analysis based on the database provided by Euronet, which contains lens orders from about 400 optical shops in Germany between the years 2000 and 2020.
Methods
Study dataset
The dataset used was obtained from Euronet (Euronet Market Research, Euronet Software GmbH, Frechen, Germany) and comprised the following variables: center identification number (and with this identification also the geographical location of the optical shop), subject identification number, purchase date, date of birth, age, gender, spectacle-plane refractive correction (sphere, cylinder, axis). The present study was in accordance with the declaration of Helsinki and all data involved in the current research were de-identified and protected by the privacy safeguards of the European General Data Protection Regulation.
Study population
Refractive data from 64,825 children aged 6 to 14 years receiving single vision lenses from 408 eye care professional (ECP) centers in Germany between 2000 and 2020 were analyzed.
Analysis
Spherical equivalent refraction (SE) data of the right eye was used for the analysis, while SE values were calculated as the sum of the sphere power with half of the negative cylinder power and children were classified as being myopic, when first purchase of spectacles indicated SE ≤ −0.50 D (SE), as described by the International Myopia Institute.12 Progression of myopia was defined as the change in prescription of the SE between the baseline visit (i.e., the first time an order was recorded in the database) and a second prescription between 11 and 24 months after the baseline visit.13 In case individuals did not meet these criteria, their data were excluded from further analysis. An annual progression of spherical equivalent below or equal to −0.50 D was defined as in need of myopia management (MM).13
Results
Number of children per shop per year
The database contained longitudinal data of n = 52,936 myopic children (SE ≤ −0.50 D) aged between 6 and 14 years who all received single vision correction. This dataset was further divided into children with an annual progression of the SE of ≤ −0.50 D as a criterion for the need of myopia management (n = 25,432) and children with an annual progression of > −0.50 D (n = 27,504), respectively. Detailed results on the number of children per shop (n = 408) and year for the two groups are displayed in table 1, separated by the age of their baseline visit.
This analysis already provides interesting insights into the current situation of myopia management in Germany. It shows that in the database analyzed, 1) there are children of all ages who require myopia management, 2) the number of kids with the need for myopia management increases with age, reaching a maximum at 10 to 11 years and declines afterwards, 3) high myopia is more frequent in younger children (6 and 7 years) when compared to children aged 9 – 12 years, 4) the number of kids that are myopic without the need of myopia management also increases with age, with highest numbers at 14 years and 5) at younger ages, there are more children requiring myopia management than children requiring myopic vision correction without the need of myopia management.
Distribution of baseline refractive errors
Table 2 shows the distribution of baseline spherical equivalent refractive error for children requiring myopia management.
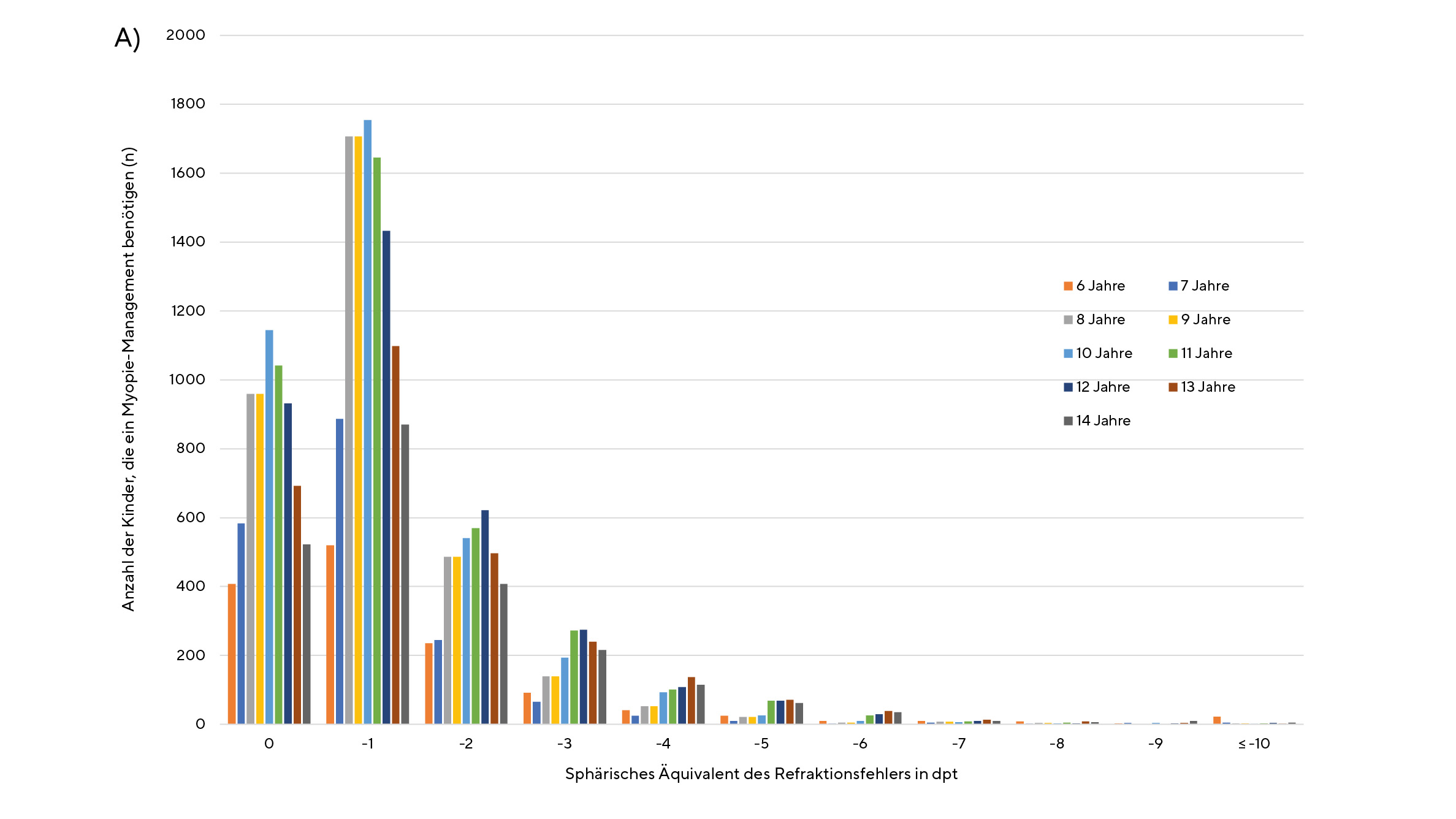
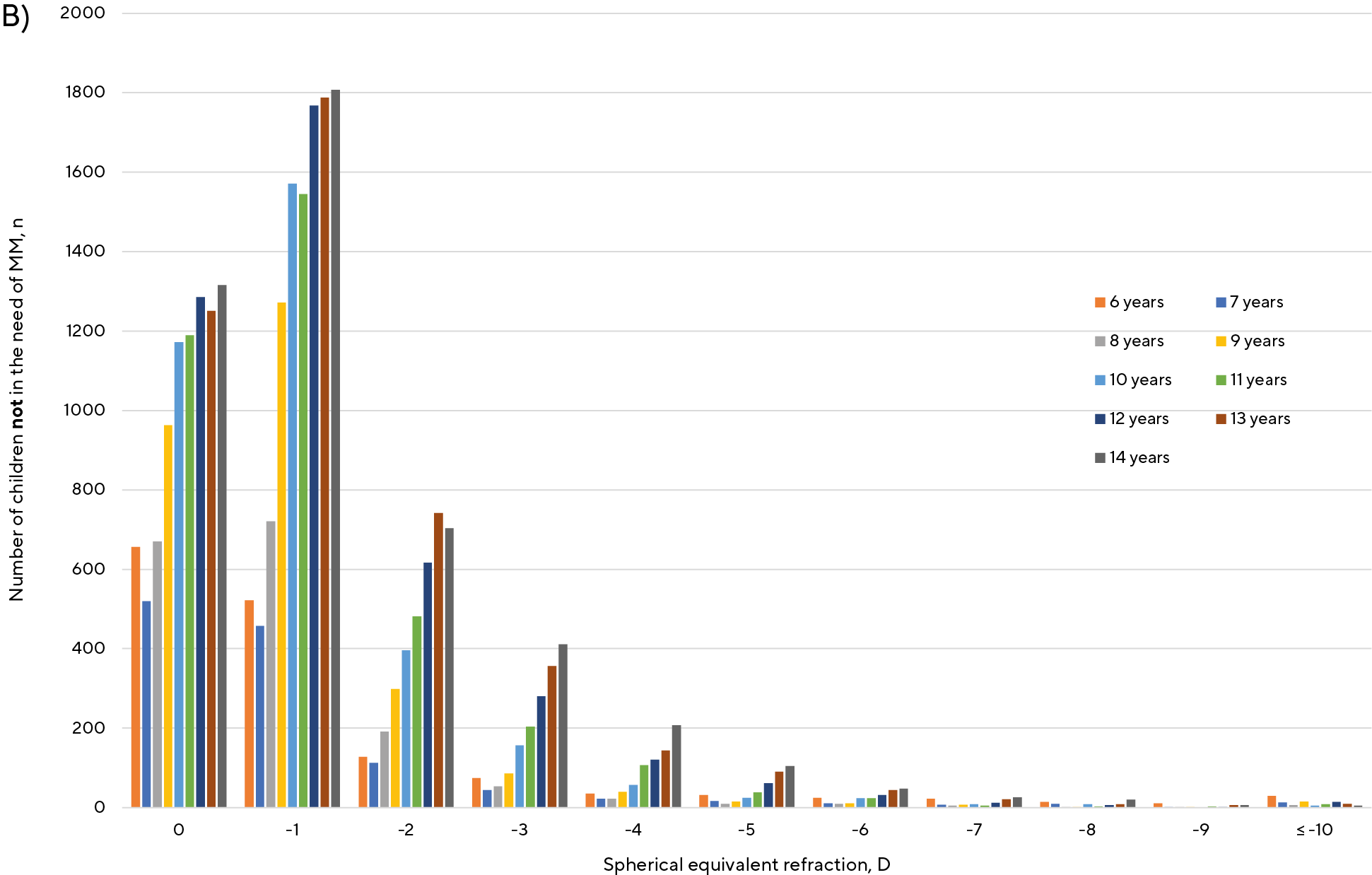
Figure 1A and 1B show that baseline refractive errors increase towards higher levels of myopia (in terms of SE) with increasing age both in myopic children with annual progression of ≤ −0.50 D (figure 1A) as well as in myopic children with an annual progression > −0.50 D (figure 1B).
Second prescription of spherical equivalent refractive error
Higher progression rates eventually result in higher levels of net myopia. Table 3 summarizes the baseline (i. e., the first record in the database) and second prescription (i. e., the follow-up record after 11 to 24 months, on average 20 months) spherical equivalent refractive error for children with an annual progression ≤ −0.50 D and > −0.50 D, respectively, as well as the average difference for each age. This analysis shows that: 1) baseline SE is very comparable between children requiring MM and children that are not requiring MM across all ages, while 2) after 11 to 24 months, SE was −0.98 D on average more negative in children requiring MM compared to children not requiring MM with a maximum difference of −1.34 D for 6-year-olds.
Pre-myopes
The database also included data on children that were not myopic at their baseline visit, but became myopic at their second prescription (i.e., the follow-up record after 11 to 24 months) with an SE ≤ −0.50 D. Analysis of their baseline and second prescription (see table 4) showed that the baseline SE was on average −0.20 D (range −0.17 D to −0.23 D), but the SE after 20 months on average ranged between −1.71 D for children at the age of 7 years and −1.29 D for children aged 14 years.
Distribution of baseline refractive errors
Table 2 shows the distribution of baseline spherical equivalent refractive error for children requiring myopia management.
Discussion
The analysis of the available data set of myopic children aged 6 to 14 years requiring myopia management gave important insights into the current clinical status quo in Germany. Below the age of 11 years, around half (47 % to 62 %) of the myopic children requiring vision correction show an annual progression ≤ −0.50 D, indicating a need for myopia management. The number of children per shop and year requiring myopia management appears to peak at the age of 10 to 11 years, while fewer children require myopia management at older ages. Further analysis on children in the need of myopia management and comparing them to age-matched children without need of myopia management showed that both groups had a similar baseline refractive error (SE average −1.68 D and −1.62 D for kids in the need and kids not in the need of myopia management, respectively), but second prescription was different by around −1.00 D (average second prescription for children with the need of MM −2.94 D vs. average second prescription of −1.94 D in children without the need of MM). The observed results reflect significant differences between children with a high versus low rate of progression and with an early onset vs. a late onset of myopia, and results are for sure influenced by the difference in progression at a younger vs. an older age. In detail, myopia progression has been shown to be highest among younger children (average annual progression of myopic children in Europe was reported to be −0.41 D for children aged 6 to 16 years and lower −0.16 D for children and adolescents aged 12 to 22 years).14 Real world evidence in France has found similar details regarding the annual progression in children aged 7 – 9 years (annual progression −0.43 D) and 10 – 12 years (annual progression −0.42 D), while the rate of progression was lower for younger and older age groups.13 It is established that children with an early onset of myopia will show higher progression rates and will consequently have a higher risk for chorioretinal diseases later in life. This additionally indicates the significant need to act early in order to effectively screen for myopic refractive errors early in life. Basic research shows that a refractive error at the age of 6 to 7 years gives the best indication if a child will develop myopia or not,15 and it could be concluded that such screening should take place at this age range or even earlier, in case of identification of myopia risks (such as parental myopia). The number of myopic children and adolescents with an baseline correction of their distance refractive error without the need of myopia management increases with age. As myopia progression decreases with increasing age, children with late onset of myopia only realize very late that they are in the need of vision correction and hence get their baseline refractive error correction later in life. All discussed results are further supported by the fact that the distribution of baseline refractive errors changed towards higher levels of myopia with increasing age, as shown in tables 2 and 3 as well as in figures 1A and 1B. The current data set covered the years from 2000 to 2020. It has not yet been analyzed how the need for myopia management has changed over this time course. Wesemann analyzed a similar database and found no evidence for an increase in the prevalence of myopia in Germany.16 In contrast, Sanz Diez and colleagues found an indication for a more myopic refractive shift in children aged 6 – 11 years in Germany, likely due to the pandemic-related home confinement during the COVID-19 pandemic.17
Data of pre-myopic children with a second prescription and an annual progression that categorizes them as in the need of myopia management suggested how to deal with such cases. While children of different ages in this analysis had very similar baseline SEs (average −0.20 D), it is interesting to note that younger children revealed again higher levels of second prescription, compared to older children. Again, this analysis shows that younger children at risk of high progression will end up with higher levels of myopia and successful myopia management needs to be considered in the daily practice of myopia management for children at (defined) risk.
.
Limitations and Potentials
Data analysis based on real-world data has not yet been widely used in the field of optometric and ophthalmic research. Such data lacks certain information such as the type of refraction techniques used (e.g., if prescription was measured with or without cycloplegia, which rule was followed during the subjective assessment of refractive errors) and most problematic: if the first visit is equivalent to the first time of use of vision correction. For example, data in table 2 indicates that sometimes, baseline refractive errors were as high as −20.00 D which is not very plausible as first-time vision correction. And as the current method of analyzing the data followed the methods as proposed by Tricard et al., the second prescription is the refractive status after only up to 24 months after the baseline correction and any further available data (i. e. change in refraction after 3, 4 or even 5 years) were withdrawn from the current analysis.13 Also further information are available in such data set, e.g. information on gender (as it is known that girls typically shower earlier onset and sometimes higher progression) or about the geographical location of the eye care professional (located in the north or south of Germany and in more urban or rural regions).
Despite these limitations, the use of real-world data will find its way into the optometric and ophthalmological practice: real-world evidence supports setting standards for the individual optometrist based on annual progression using a certain method of intervention (spectacle lens, soft contact lens, Ortho-K) and is already implemented into regulatory decisions. Additionally, future analysis of sales of myopia management solutions based on either the type of intervention (spectacle lens, soft contact lens, Ortho-K, pharmaceutical solutions) or the mechanism of action, based on network management software or based on industrial manufacturing database will further give important insights into the needs and the status of myopia management in Europe and other regions.
Conclusions
The present analysis suggests that screening for (especially myopic) refractive errors is not performed satisfactorily, as only a small number of myopes are present at the eyecare professional at a young age.
Acknowledgment
With kind support of the Market Research Division of Euronet Software GmbH.
Conflict of Interest
All authors declare that they are employees of Carl Zeiss Vision International GmbH or Carl Zeiss Vision GmbH, as indicate by the personal affiliation.
myopia control? Education and other barriers to the treatment of
myopia. HRB Open Res., 23, 2:30.
a nationwide longitudinal study. Br. J. Ophthalmol., 106, 1104–1109.
