Changes in the NPC in patients with convergence insufficiency after I.F.S. visual therapy
Purpose: The aim of this study was to evaluate the efficacy of the I.F.S. visual therapy (convergence training), developed by Bruce Evans, in a randomised-controlled setting. The main objective of the study was to analyse the changes in the near point of convergence (NPC).
Material and Methods: 20 subjects (39.0 ± 15.32 years) with convergence insufficiency and an NPC > 10 cm underwent 4 weeks of convergence training in a randomised-controlled, single-blind setting. The verum group performed I.F.S. exercises, while the control group underwent a placebo training. Before and after the training phase, the NPC and the positive fusional vergence (PFV) were measured in all subjects and the Sheard and Mallet criteria assessed. The CISS (Convergence Insufficiency Symptom Survey) was used to record and quantify subjective symptoms.
Results: The statistical analysis (α=0.05) shows that the NPC of the verum group improved significantly compared to that of the control group (p=0.0008), also when considering the test group only (p=0.0002). The positive effect of the I.F.S. exercises was also confirmed by the significant improvement in PFV.
Conclusion: The results as well as the practical experience with the exercises indicate that the I.F.S. visual therapy proves to be effective in improving the near point of convergence in individuals with convergence insufficiency and an NPC > 10 cm.
Introduction
Convergence insufficiency (CI) can be the cause of headaches or drowsiness that quickly occur while reading, can make letters sometimes appear blurry and rapidly reduce the concentration and text comprehension when reading longer texts. This binocular abnormality affects 3% to 8% of society1 and manifests itself through an increased near point of convergence (NPC)2, a greater exophoria for short distances compared to long distances1, a reduced positive fusional vergence (PFV)3, and a low AC/A ratio. The latter describes by how many prisms the eye position changes due to convergence per diopter of accommodation.3 However, it only makes sense to record this ratio when examining pre-presbyopic test subjects, since presbyopia reduces accommodation and renders this value meaningless.3
The preferred therapy for convergence insufficiency is visual therapy (VT) to improve convergence ability. This therapy iscomposed of various exercises tailored to the patient's problems.1,4 The series of exercises are completed either at home (home-based) or in a clinic under the supervision and instruction of an optometrist/ophthalmologist (office-based). Sometimes the training can also be performed as a combination of the two possibilities. The simplest type of visual therapy is the "pencil push-up treatment" (PPT), in which an accommodative object (e.g. a pencil tip) is held in front of the patient's eyes at arm's length and then approximated.1,4 Throughout the period of approximation, bifoveal fixation should be maintained until diplopia is observed. The described procedure is used by many practitioners because it is easy to perform and is therefore well suited for independent, home-based training. The CITT group (Convergence Insufficiency Treatment Trial) conducted several studies to evaluate the effectiveness of various visual therapies, including the PPT. The latter turned out not to be much more effective than placebo therapy.5 Another study performed by the group found that office-based VT leads to statistically significant improvements in NPC and PFV – but not PPT alone.4,5 Home-based training, which consists of other exercises in addition to PPT, such as stereograms, the brock string, exercises with eccentric circles, etc., is much more successful and shows good results. However, in order to be effective, the supervising specialist must give detailed explanations, a fact which can lead to the exercises being less effective when carried out at home compared to in-office training under supervision.4 Patients who don't have the time for an intensive in-office training can now undergo visual therapy using a computer.4 The HTS (home therapy system) Vergence and Accommodation is a simple program that uses random-dot stereograms to perform visual therapy and adapts the difficulty levels of the exercises to the progress of the patient.1
Vaegan noted that the key to a successful visual therapy is to maintain extreme convergence over longer periods of time.6 Extreme convergence is defined as the vergence of the eyes at an angle between the break point and the recovery point that can only be maintained with a certain degree of effort. Vaegan also mentioned that it does not matter if a synoptophore or cards with stereograms are used for training, but that rather the above-mentioned persistent extreme convergence is a decisive factor. In order to motivate the patients and prevent boredom, exercises for CI therapy should be as varied and interesting as possible, as is the case with the I.F.S. exercises examined in the present study.6
The I.F.S. visual therapy (Institute Free-Space Stereogram exercises) was developed by Bruce Evans, who evaluated its efficacy in 2000 as part of a non-blinded, open trial study.7 The results were promising, as the NPC and other values of the subjects could be significantly improved. However, Evans noted that a study of the I.F.S. VT in a randomised-controlled setup would be desirable7, as this is considered the preferred study design to investigate a medical therapy and its effect on a defined target value. Another advantage of a randomised setting with a verum and control group is that systematic differences between the groups can be largely excluded. Thanks to the additional simple blinding, the subjects do not know whether they are performing the I.F.S. or the placebo therapy. This makes it possible to record a potential placebo effect within the control group.
Material and Methods
This study complies with the principles of the Declaration of Helsinki, received the approval of the Ethics Committee of Northwestern and Central Switzerland EKNZ (BASEC: 2018-00087) and is registered in the German Register of Clinical Trials DRKS (Study ID: DRKS0001487).
Menjivar et al. compared different procedures such as measuring the NPC, determining PFV and recording the CISS score and tested their suitability as screening methods. The measurement of the NPC was found to be the best regarding sensitivity and specificity and was declared the preferred screening method for the detection of convergence insufficiency.8 The main inclusion criterion in the recruitment of test subjects was therefore an NPC > 10 cm, measured at eye level and from the nasal bridge.
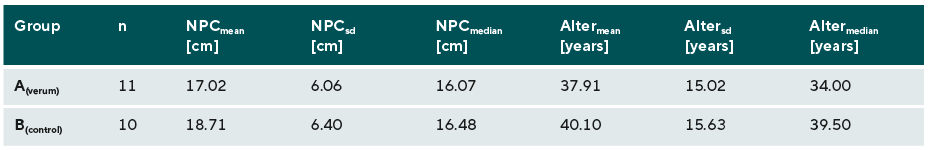
The 20 participating subjects (39.0 ± 15.32 years), all of whom had no systemic diseases, were homogeneously distributed in the NPC and age, and randomly divided into a verum and control group (n = 10 each). The I.F.S. VT assumes that patients can perceive a spatial depth on the exercise cards with a correct convergence, which is why people with strabismus or non-intact stereoscopic vision were excluded from the study.
The training time in both groups was 10-15 minutes daily for 4 weeks. The verum group performed the I.F.S. VT, while the control group completed a placebo therapy, which was designed in such a way that the exercises did not train convergence in any way. All subjects had a diary to document their training.
I.F.S.-Visual Therapy
The I.F.S. exercises developed by Bruce Evans consist of 4 cards in A4 format and a training manual. Integrated into the exercise series are 10 self-assessment questions which indicate the patient, depending on the answer, whether the training is being carried out correctly. The cards and the exercises are structured in stages, so that the patient is gradually guided towards the goal and has the opportunity to repeat the steps until a learning curve can be established. The training uses 3D elements and is designed to be interesting and varied for the patients, since it aims at increasing the patient's compliance. This leads to the eyes of the test subjects being in extreme convergence for a long time, meaning that the therapy should show positive results despite being performed over a relatively short time span.7
When carrying out exercises to train fusional vergence, there are various options for dissociating the eyes, with I.F.S. VT using free-space-fusion with random dot stereograms.2,7
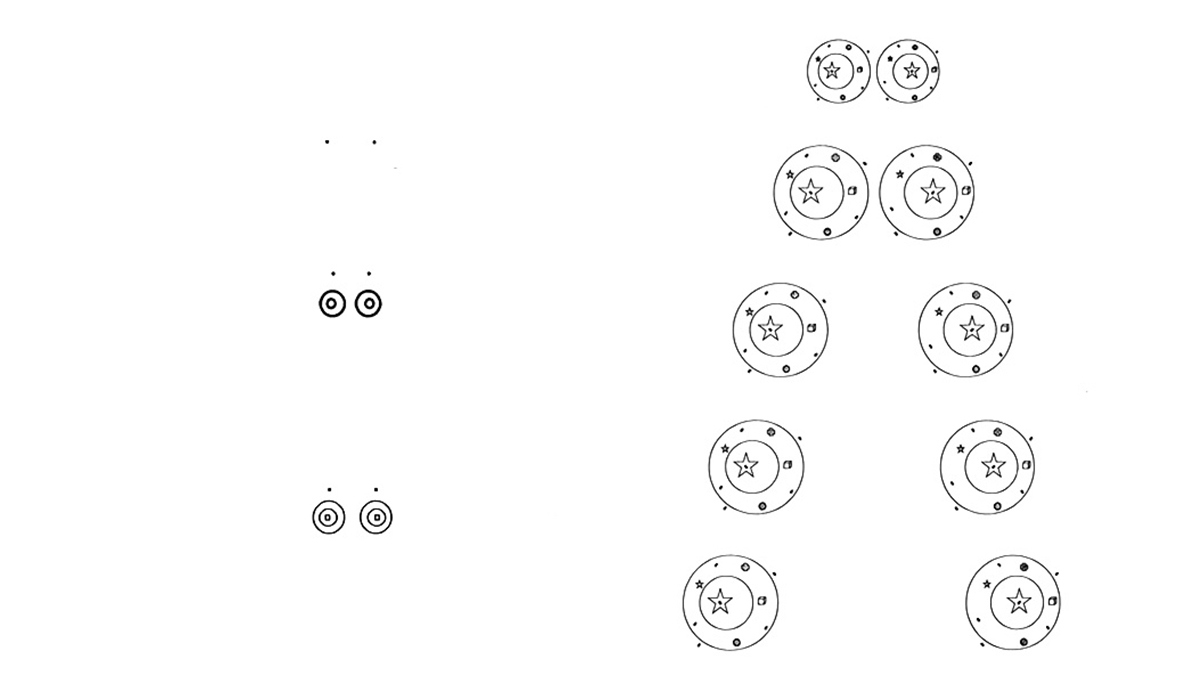
The exercises on the first card show the patients how they can use physiological double vision to create stereopsis. The patients will already perceive stereopsis with the exercises on this card, but only a slight extreme convergence is necessary for this.2 Figure 1 shows the design of the first two cards.
Card 2 not only trains extreme convergence, but also uses various techniques that help the patients improve their convergence and stereoscopic perception. In a first step, various exercises are used to increase sensory perception. Later, the patients learn to recognise differences in depth in stereoscopic vision, to differentiate them from one another and to describe them. The further down the pairs of rings are on the card, the further apart the two associated rings are and the more positive relative convergence is necessary to be able to achieve stereopsis.7
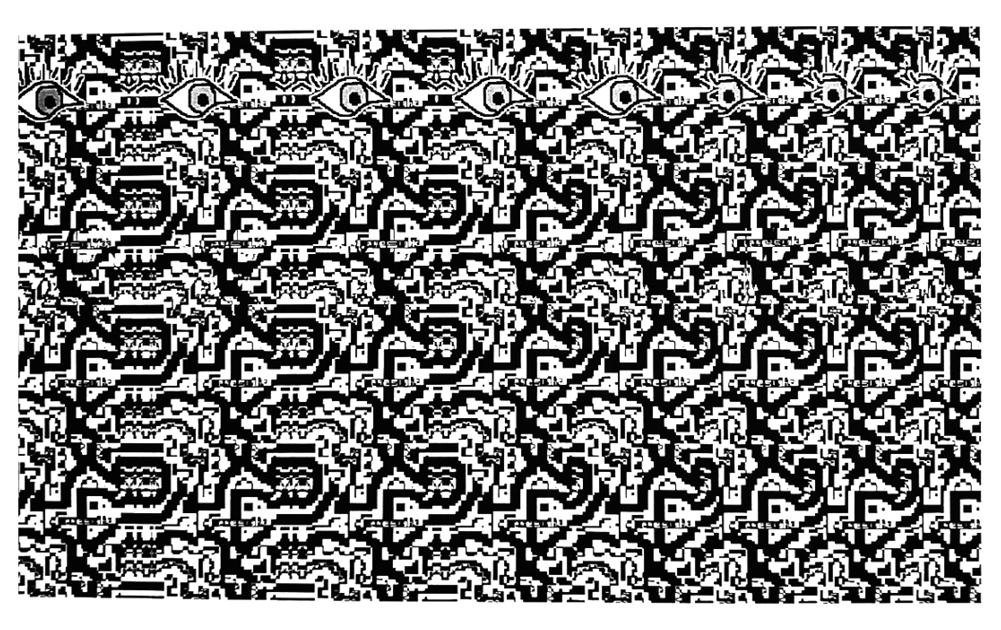
The third card of the training, as shown in Figure 2, shows a random dot autostereogram. If the exercise is carried out correctly, the patients can see a staircase that comes towards them with each step and thus demands increasing convergence. Card 4 is also an autostereogram but with a slightly more difficult structure.2,7
Measurement methods
The main aim of the study was the analysis of the change in the NPC (main inclusion criterion), which was measured using a video-based, free-space measurement method (Sony Digital HD, HDR-TG1E) before and after therapy by approaching a pencil tip towards the nasal bridge. The subjective and objective break points were then recorded.9 The subjective break point is defined as the point at which the patient specifies that he or she sees the close-up object double. In the case of the objective break point, the examiner observes the patient and notes when one eye stops converging and deviates. Out of the two maximum break points, the first one to occur is the most relevant.10 If a measurement cannot be taken without glasses, the measured value is then adjusted using a correction table to counteract any possible prismatic side effects.9
Additionally, the PFV, the CISS score and the Sheard and Mallett criteria were also recorded and analysed before and after therapy. The data were checked for changes between before and after therapy within the two groups as well as for differences between the verum and the control group. However, the main focus was on the analysis of changes in the NPC.
The measurement of the positive fusional vergence, i.e. the convergence fusional reserve with constant object distance, was carried out with a fixation object at 40 cm on the phoropter while steadily raising the prism power base out. The standard value for the break point is defined in the literature as 21 ± 6 cm/m; this value is often smaller in the case of convergence insufficiency.3
The Sheard criterion is connected with near exophoria and is fulfilled when the blur point of the PFV at short distances, i.e. the convergence fusional reserve, is twice as large as the exophoria at short distances.2 The fulfilment of this criterion ensures that the patient can comfortably compensate for the phoria through convergence or divergence, even over a longer period of time and neither perceives a blurred nor a double image.1 The measurement of the dissociated near phoria necessary to determine the Sheard criterion was carried out with the Thorington test card in combination with the Maddox rod. Since this test is performed at a distance of 40 cm, a direct comparison of the phoria with the previously measured positive fusional vergence is possible. However, it is not only of interest whether the criterion is met or not, but also how large the measured deviating prism power of the Sheard criterion is. If the deviating prism power is positive, the criterion is fulfilled. If, on the other hand, the prism power is negative, the criterion is not fulfilled.
The Mallett test is an associated test with central fusion stimulus and can indicate fixation disparity, which usually occurs in sensory, poorly compensated heterophoria.11If the test subjects perceive the test figures to be shifted from one another, the lowest possible prism power, the aligning prism, is used so that the test appears centred. The Mallett criterion is fulfilled if the prism correction is less than 1 cm/m for pre-presbyopic patients and less than 2 cm/m for presbyopic patients.2 For the present study, the numerical value of the mentioned prism correction was used for the statistical analysis, which enables an additional analysis about a possible change in the value thanks to the VT.
Subjective present symptoms can be quantified with the CISS (Convergence Insufficiency Symptom Survey) consisting of 15 questions. The limit value for adults with symptomatic CI is 21 points.4
The measurement of the AC/A ratio was omitted because the group examined included pre-presbyopic and presbyopic subjects.
Statistical analysis
The statistical evaluation was carried out using Microsoft Excel and the Rcommander statistics program (Rcmdr, version 3.2.2). The data were checked for normal distribution with the Shapiro-Wilk test and for statistical significance with the t-test for independent samples or the Wilcoxon test, in the case the values were not normally distributed. The correlation between NPC and PFV was evaluated using the Pearson correlation coefficient. The significance level was α = 0.05.
Results
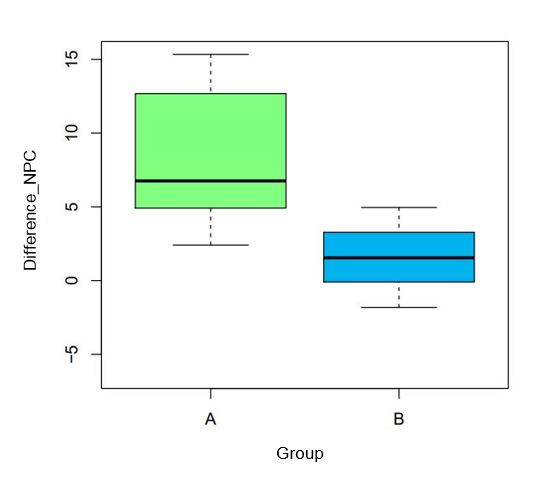
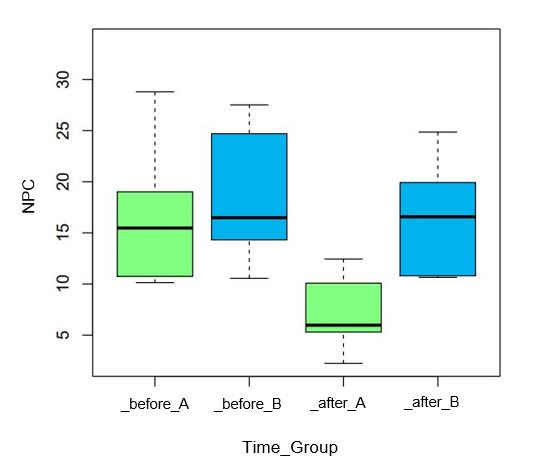
The descriptive statistics for the initial values after homogeneously distributing the test subjects in the NPC and age can be found in Table 1. Figure 3 depicts how the statistical analysis of the data (α = 0.05) shows that the difference in the NPC (cm) of the verum group (group A, green) before and after training differs significantly (p = 0.0008) to the difference before and after therapy in the control group (group B, blue).
The positive effect of the I.F.S. visual therapy is also supported by the analysis of the verum group alone, in which the mean improvement in the NPC is 8.12 cm (± 4.37) and is also statistically significant (p = 0.0002). Within the control group, the improvement in the NPC is only 1.04 cm (± 3.31) and is not significant (p = 0.3452). Figure 4 shows the NPC values before and after the four-week therapy separately for groups A and B, demonstrating the aforementioned results again.
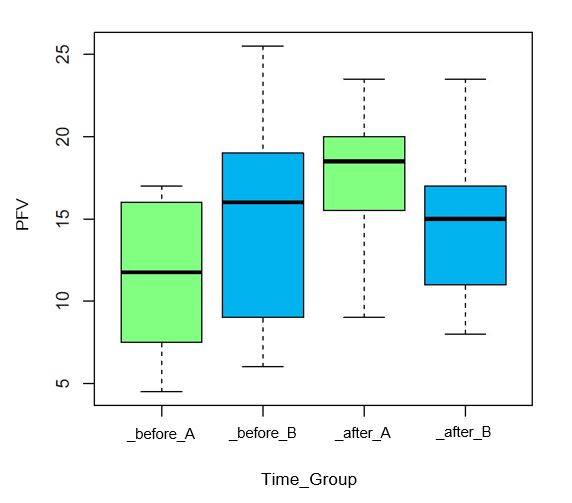
Figure 5 shows the values of the PFV (cm/m) before and after therapy separately for groups A and B. It can be seen that the PFV of the test subjects in the verum group has changed to a greater extent and has improved compared to the control group. This change in the difference between before and after the VT between the two groups is significant (p = 0.0013) and is confirmed by the statistically significant (p = 0.0013) average improvement of 4 cm/m (± 4.41) within the verum group. Within the control group, this change was 0.1 cm/m (± 2.02) and is not statistically significant (p = 0.8739).
The correlation between NPC and PFV was checked using the Pearson test assuming a normal distribution of the difference values; it gave a correlation coefficient of r = 0.81, which is statistically significant (p < 0.0001). Both groups are represented in this evaluation, and it can therefore be said that, on the one hand, the significant improvements in the values of group A correlate, and, on the other hand, the non-significantly changed values with regard to NPC and PFV of group B also correlate.
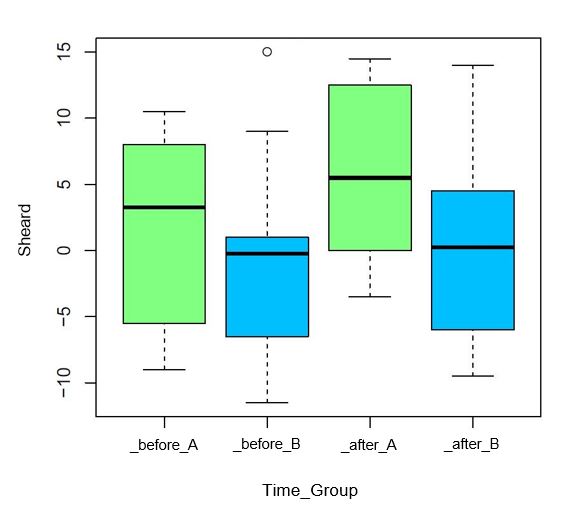
The analysis of the subjective symptoms (CISS score) and of the values of the Mallett criterion did not reveal any significant changes in either the verum or control group or in the comparison of the two groups. In the verum group, a mean improvement in the values for the Sheard criterion of 4.20 cm/m (± 3.95) was found to be statistically significant (p = 0.0084), which is also evident when looking at the number of test subjects that met the criterion. Before the I.F.S. VT was carried out, 6 out of 10 subjects in the verum group met the criterion, while 9 out of 10 fulfilled it after the four-week training. In the control group, on the other hand, the number of subjects who met the criterion only increased from 4 to 5. The graphic representation of these changes is shown in Figure 6.
Discussion
The main aim of the present study was to find out whether there was a difference in the change in the NPC before and after therapy between a group performing I.F.S. VT (verum group) and a group performing a placebo therapy (control group). Since the statistical analysis of this main hypothesis showed a significant difference, and because there was a clinically relevant change in the NPC by an average of 8.12 cm, it can be concluded that the I.F.S. VT significantly improved the NPC and, thus, the convergence ability of convergence insufficient patients. If the two groups are considered starting from the definition of CI given in this study (NPC > 10 cm), only 3 of the 10 test subjects in the verum group can still be considered to have a convergence insufficiency after the therapy was carried out, whereas the whole control group remained insufficiently convergent (10 out of 10).
These results would be even more robust if the subjective discomfort had also been reduced at the same time. However, there was no significant improvement in the CISS score recorded immediately after the training phase. It was difficult for the test subjects to assign scores in the CISS right after therapy, since they did not have enough time to get acquainted with the new situation after the second measurement. This resulted in the patients mixing their experience before, during and after therapy when filling out the CISS. Therapeutic effects can best be recorded using symptom diaries, which, however, at the same time increases the drop-out rate of the participants.12 The fundamental significance of the CISS score with regard to CI is critically discussed in the literature. For example, Marran et al. found no significant difference in the score between children with convergence insufficiency and children with normally developed binocular vision13, whereas a study by Rouse et al. lists a significant difference in the analysis of the CISS score.14
Regarding the Sheard and Mallett criteria, Evans found significant results which could only be partially confirmed in the present study. The likewise statistically significant change in the prism value for the Sheard criterion could be expected due to the associated improvement in the PFV in the verum group.
The values resulting from the evaluation of the Mallett criterion were statistically difficult to evaluate, since only 2 test subjects in the verum group and 5 in the control group showed a fixation disparity in the initial measurement. Out of these, only one test subject in the verum group and 2 in the control group did not meet the criterion. This result was to be expected because it often happens with the Mallett test that the tested person sees the nonius lines aligned and therefore does not exhibit a fixation disparity. Karania and Evans did not find any horizontal fixation disparity in 80% of their test subjects (n = 105) when they only asked about the position of the nonius lines. Only when they also asked about their displacement and movement did the rate change to 61%.11
For the reasons mentioned above, no meaningful conclusion can be drawn as to whether the I.F.S. therapy has a positive effect on people with fixation disparity. A larger number of test subjects or expanded inclusion criteria regarding fixation disparity could provide more information on this aspect.
Carrying out the I.F.S. therapy proved to be demanding, and the majority of the test subjects initially had to hold a pencil between their eyes and the exercise card to aid convergence. However, as soon as the principle of extreme convergence was clear and the test subjects experienced a sense of achievement when performing the exercises, motivation rose again. The good compliance of the test subjects certainly contributed to the significant improvement of the NPC in the verum group, whereby it should be noted that those test subjects who did not exercise daily also experienced a similar improvement. This suggests that it is not just the training time and the number of exercises completed, but mainly the duration of extreme convergence that contributes to the success of the visual therapy, as Evans had already stated.7 This hypothesis is supported by the fact that the majority of the test subjects needed a pencil as a convergence aid during the entire training period, resulting in the eyes being in constant extreme convergence, even if the execution of the exercise in question was not yet fully functional. Cooper et al. showed as early as 1983 that patients with convergence insufficiency must first learn to stimulate convergence before carrying out visual therapy, as shown here, for example, with a pencil as an initial convergence aid.15
If the exercises are carried out correctly, 3D elements become visible on all I.F.S. VT cards, something which kept the test subjects' motivation high and ensured a noticeable sense of achievement. The random dot autostereograms are particularly demanding, but also stimulating, as the test subject wants to know which 3D elements are hidden behind the pattern. A study by Cooper and Feldman showed that working with random dot autostereograms improves the ability to converge to a greater extent than training with conventional vectograms, and that what is learned can be better transferred to "everyday vision".16 A direct comparison of the results of the aforementioned study and the present one is only possible to a limited extent, however, since Cooper and Feldman let the test subjects train in-office under supervision and not independently at home, as is possible with the I.F.S. VT.7,16
In conclusion, it can be stated that I.F.S. VT, if carried out correctly, leads to a rapid improvement in the convergence ability in patients with convergence insufficiency. With regard to the representativeness of this conclusion, it should be noted that this is only guaranteed for adults with an NPC of over 10 cm (main inclusion criterion) and only to a limited extent, as further influencing factors could not be taken into account due to the reduced number of test subjects of this study. In order to ensure better representativeness, which would allow for the analysis of further factors and thus the projection of the results onto a larger population, a study with a larger number of subjects using diaries to record their symptoms would be advisable.
Conclusions
The present study confirms and reinforces the results of the open trial study2 carried out by Bruce Evans by performing the visual training in a randomised-controlled setting. Although studies with more test subjects would lead to a higher representativeness, it can be stated that the I.F.S. visual therapy is well suited as a convergence training and leads to a significant improvement in the ability of affected individuals to converge and requires comparatively little time both for the patient and the optometrist.
Conflict of interest
The authors have no conflict of interest regarding the methods and devices mentioned in this article.
COE Multiple Choice Questionnaire
The publication "Changes in the NPC in patients with convergence insufficiency after I.F.S. visual therapy" has been approved as a COE continuing education article by the German Quality Association for Optometric Services (GOL). The deadline to answer the questions is 1 December 2022. Only one answer per question is correct. Successful completion requires answering four of the six questions.
You can take the continuing education exam while logged in.
Users who are not yet logged in can register for ocl-online free of charge here.
