Ocular Inflammation Associated with Sarcoidosis: Anterior Uveitis, Vitritis and Macular Edema
Purpose. Sarcoidosis is a chronic inflammatory disease that can affect the eyes, lungs and skin and other organs in the body. Ocular sarcoidosis can include: uveitis, episcleritis, scleritis, conjunctival granuloma, lacrimal gland enlargement, optic neuropathy and retinal and orbital inflammation. The aim of this article is to highlight a case of ocular sarcoidosis and to discuss the diagnosis and appropriate treatment options.
Material and Methods. A patient with a history of sarcoidosis presented with complaints of pain, decreased vision and glare. Evaluation revealed a diagnosis of unilateral anterior and intermediate uveitis and macular edema. The patient was educated on the potential treatment options and the decision was made to treat with topical anti-inflammatory drops. The patient was co-managed with their pulmonologist.
Results. Topical anti-inflammatory treatment successfully resolved all aspects of the patient’s ocular inflammation. However, it is crucial to be aware of all potential treatment options, methods of delivery and to involve the patient in their treatment plan.
Conclusion. Sarcoidosis can affect multiple organ systems including the eye. This article discusses the diagnosis and treatment of a patient with ophthalmic manifestations of sarcoidosis. Optometrists can play a key role in diagnosing and treating ocular manifestations of systemic disease.
Introduction
Sarcoidosis is a chronic and systemic inflammatory disease of uncertain cause. It has been postulated that it is caused by exposure to antigens causing an immune response that leads to collections of cells called granulomas. Specifically, these non-caseating granulomas do not contain dead or necrotic cells.3 The formation of these non-necrotizing granulomas seems to occur in certain patients with a genetic predisposition to create this immune response. Epidemiologically, certain ethnic African and Scandinavian groups have a higher incidence of sarcoidosis.4 Chronic inflammation in various organ systems can lead to scarring and irreversible damage, especially in the lungs, eyes, heart, kidneys, liver, and spleen. Symptoms vary in type and severity but can include cough, shortness of breath, lymphadenopathy, joint pain, eye pain and blurred vision, skin rash, among others.3
Imaging tests and biopsy of the involved organ aid in the diagnosis.5 Sarcoidosis can affect any part of the eye, with the most common ocular manifestation being uveitis.6 The chronic ocular inflammation can lead to significant damage to the eye, making timely diagnosis and treatment imperative.
Case Presentation
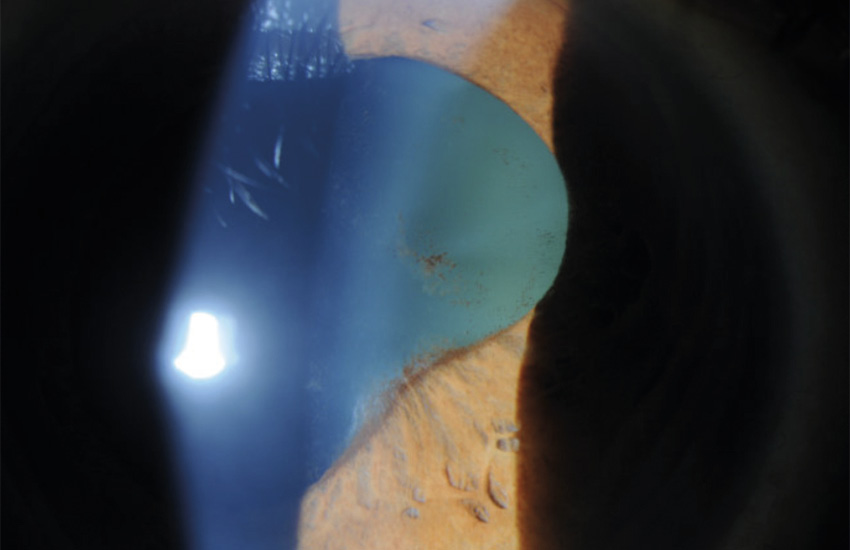
A 57 year-old female presented to our clinic with complaints of blurry vision, glare and dull pain in the right eye x 1 month. The patient has a history of sarcoidosis and admits to neglecting their appointments with their pulmonologist. The patient reported that they were currently not taking any medications. They do not report any chest pain or difficulty breathing. The exam findings are as follows: Uncorrected visual acuity was: 20/40 OD, 20/20 OS and refraction does not improve vision in the right eye. Pupils were equal, round, reactive with no APD. Extraocular motilities were full and confrontational visual fields were full to finger counting in each eye.
Cirrus spectral domain optical coherence tomography (OCT) (5 line raster and 512 × 128 macular thickness scans) of the macula were performed which confirmed the cystoid macular edema of the right eye with no choroidal thickening. (Figure 2). The OCT of the left eye revealed a normal macula and choroid.
Our patient was diagnosed with anterior uveitis, intermediate uveitis and macular edema associated with systemic sarcoidosis. Treatment options were discussed which included topical and intraocular injections and their potential side effects. The patient was resistant to be treated with an injection and preferred that a non-invasive treatment be attempted first. They were prescribed prednisolone acetate ophthalmic suspension 1% q4h OD, ketorolac 0.4% ophthalmic solution QID OD and cyclopentolate ophthalmic solution 1.0% BID OD and told to return in 1 week for follow-up. The patient was educated that an intraocular injection would be offered to treat the cystoid macular edema if there was an inadequate response to the topical therapy. Our findings were communicated with their pulmonologist and they were educated on the importance of follow-up.
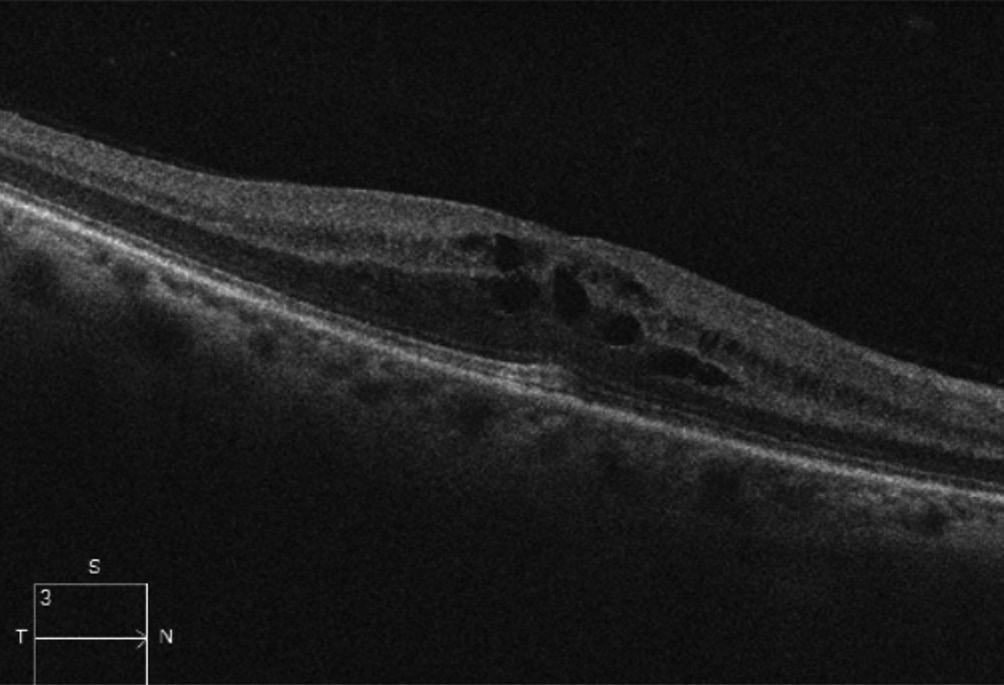
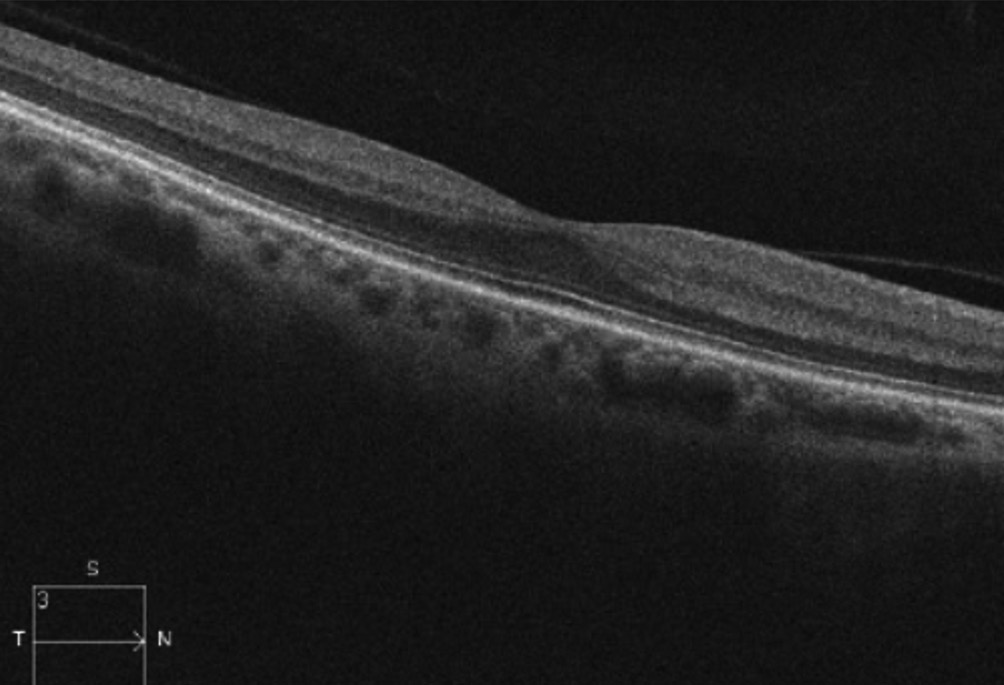
Our patient’s signs and symptoms improved on all visits and we started to taper the prednisolone and ketorolac. At the 5 week follow up the vision in the right eye improved to 20/25 +. Trace cells were noted in the anterior chamber, and no cells were noted in the vitreous. The posterior synechiae persisted. Intraocular pressure was stable in each eye. The cystoid macular edema resolved in the right eye as shown in Figure 3 on the OCT scan of the macula. All topical medications were eventually discontinued.
Discussion
Ocular involvement is present in approximately 10-55 % of patients with sarcoidosis.7 Although sarcoidosis can occur anywhere in the eye, the most common ocular manifestation is uveitis, which can be anterior, intermediate, posterior or panuveitis. Anterior uveitis with bilateral involvement is the more common presentation and granulomatous in nature reflected by the presence of mutton-fat keratic precipitates.7 There are other granulomatous disease such as tuberculosis and syphilis that may show similar inflammatory reactions. Additionally, the presence of iris findings from the pupillary border to the iris root include Koeppe, Bussaca and Berlin nodules.8 Intermediate uveitis often reflects a characteristic “string of pearls” appearance of the vitreal cells.5 Common symptoms are pain, light sensitivity and decreased vision.
Less commonly, posterior uveitis can present. This may involve a nodular or segmental periphlebitis, with irregular granulations around the retinal vessels, referred to as “candle wax drippings”.7 In addition, retinal microaneurysms, choroidal and optic disk granulomas may be present.7 Chronic uveitis can lead to cataract formation, glaucoma, and cystoid macular edema (CME).9 Other possible ocular manifestations include but are not limited to dry eye secondary to lacrimal gland infiltration, band keratopathy, conjunctival nodules, scleritis, iris synechiae, and choroidal granulomas.10 Biopsies of the eyelid and conjunctival may be helpful for sarcoidosis diagnosis being that these are more accessible and less invasive than a lung biopsy.10 Neurosarcoidosis can lead to cranial nerve involvement, specifically in the facial and optic nerve, with possibility of papilledema, nystagmus, and visual field defects.11
There are reported sarcoidosis syndromes associated with ocular manifestations. Heerfordt’s syndrome is a sarcoidosis syndrome in which the parotid gland is infiltrated. The 7th cranial nerve runs through the parotid gland, resulting in a seventh nerve palsy coupled with an acute uveitis.12 Another important syndrome is Lofgren’s syndrome which includes fever, erythema nodosum, bilateral hilar adenopathy and acute uveitis.1
A general work up for sarcoidosis should include a chest x-ray or chest CT looking for hilar lymphadenopathy.5 Other testing can include angiotensin converting enzyme levels (ACE), serum lysozyme, and lung function tests conducted by pulmonology. Although definitive diagnosis would require biopsy, these tests can be supportive.13 In those patients who are unable to tolerate biopsy, bronchoalveolar lavage can be helpful. The aspirate from this technique is analyzed for the CD4/CD8 ratio which tends to be higher in sarcoidosis. It is important to know that in cases of pediatric sarcoidosis, ACE levels in normal children are generally higher than in adults and there is no reference value for children.1 Also, ACE inhibiting blood pressure medications can mask elevated ACE levels so will be of no value in patients taking these
medications.1
While treatment of ocular manifestations of sarcoidosis (especially uveitis) typically includes corticosteroids as the mainstay of treatment, there may be a challenge in choosing the appropriate management, especially in patients with CME. It is important to note that corticosteroids can be administered as topical drops, injections, implants, or orally.14 There are several case dependent factors to consider when determining appropriate treatment options. For example, topical drops are typically used for mild to moderate presentations and for anterior segment involvement. An ocular injection is typically considered when there is posterior segment involvement and the presentation is more severe or if the topical drops are not adequately treating the inflammation. Intraocular and periocular injections typically include triamcinolone acetonide, dexamethasone or fluocinolone acetonide and have greater bioavailability as compared to topical and oral routes of administration. It should be noted that there is an increased risk of complications such as infection and hemorrhage. A dexamethasone pars plana implant is another option, especially in those with recurring macular edema.15 Short courses of systemic corticosteroids may be considered in chronic, bilateral uveitis, or those who respond poorly to first line local ocular therapies. Other ocular treatment options include topical carbonic anhydrase inhibitors, and intravitreal anti-VEGF (anti vascular endothelial growth factor) injections.16 When uveitis and CME are refractory to first line local therapies, long term systemic immunosuppression therapy may become necessary. This requires co-management with a uveitis specialist, rheumatologist or pulmonologist. Second line systemic immunosuppressive agents include methotrexate, mycophenolate mofetil, azathioprine and cyclosporine.17 Third line treatment options include biologic agents which are Tumor Necrosis Factor (TNF)-α inhibitors. These may prevent systemic and ocular granulomatous inflammation.17 It is important to recognize that systemic side effects may occur with each of these treatment options and these patients must be systemically surveilled by these subspecialists.
Conclusions
Sarcoidosis can affect multiple organ systems including the eye. There are multiple ocular manifestations with anterior uveitis being the most common. This case represents a patient with a unilateral inflammation involving the anterior and posterior segment of the eye with a known diagnosis of sarcoidosis. This patient was successfully treated with topical anti-inflammatory drops. However, it is crucial to be aware of all potential treatment options, methods of delivery and to involve the patient in their treatment plan. Patients should be educated that the use of steroids may be associated with secondary glaucoma and cataracts with prolonged use.18 Patients with ocular inflammation associated with sarcoid should be monitored carefully for recurrences and co-management is essential. Our diagnosis prompted this patient to reinstate care with her pulmonologist. Optometrists can play a key role in diagnosing and treating ocular manifestations of systemic disease.
Conflict of interest
The authors declare that there is no conflict of interests regarding the methods and devices mentioned in the article.
COE Multiple Choice Questionnaire
The publication "Ocular Inflammation Associated with Sarcoidosis: Anterior Uveitis, Vitritis and Macular EdemaL" has been approved as a COE continuing education article by the German Quality Association for Optometric Services (GOL). The deadline to answer the questions is 1.April 2026. Only one answer per question is correct. Successful completion requires answering four of the six questions.
You can take the continuing education exam while logged in.
Users who are not yet logged in can register for ocl-online free of charge here.
(2023). Ocular sarcoidosis in adults and children: update on clinical manifestation and diagnosis. J. Ophthalmic Inflamm. Infect., 13, 41.
Isaac, S., Boussel, L., Calender, A., Androdias, G., Valeyre, D., El Jammal, T. (2021). Sarcoidosis: A Clinical Overview from Symptoms to Diagnosis. Cells, 10, 766.
323-345.
