Orthokeratology for high myopia
Purpose. With an increasing proportion of children with myopia especially in Asia, efforts have been made to reduce chances of preventable sight loss related to high myopia in the future. Orthokeratology lens has been used as one of the modalities not just to correct myopia, but also to slow down myopic progression and axial elongation. This case report reviews a patient with clinically significantly high myopia, whose refractive errors was partially corrected with orthokeratology lens and spectacle lenses.
Material and Methods. A now 14-year-old patient with a history of fast progressing myopia, was prescribed and commended orthokeratology to manage myopia, while regularly monitoring her refractive errors, axial length, binocular
vision status, corneal topography, and anterior eye health was
monitored regularly at the author’s practice.
Results. Over a two year follow up period, a partial correction of high myopia with orthokeratology lenses and residual refractive errors with additional spectacle lenses was effective in managing this patient’s myopia, as well as slowing of axial elongation. An updated pair of orthokeratology lens with a steeper back optic zone radii were prescribed to reduce superficial corneal staining and to maintain corneal health.
Conclusion. Patient commitment and adherence to close monitoring of eyes in terms refractive errors, axial length, and anterior eye health, are vital in achieving a successful orthokeratology lens wear for high myopia. A dual fitting strategy consisting of orthokeratology lens and spectacle wear can be a safe management strategy that is acceptable for patients with high myopia. It would be helpful for practitioners to be able to rely on robust evidence-based guidance when determining whether lens wear can be ceased, i.e. when further axial elongation and myopic progression are no longer likely.
Background
It has been predicted that half of the world’s population would be myopic by 2050, and among those with high myopia, many are at risk of preventable sight loss.1 A lot of effort has been devoted to clinical management of children with myopia as young as six years old, especially in Asia, with the use of ophthalmic spectacle lenses, contact lenses or therapeutic agent.2,3,4 Studies have shown that orthokeratology (orthoK) lenses could effectively slow down progression of axial elongation and thus myopia, and in children, especially in low to moderate myopia.4,5,6,7
The principle of orthokeratology lenses involves several changes at the corneal epithelium and stroma. The lens exerts hydraulic forces onto the central cornea via the tear film, causing a so-called epithelial shift. This causes the central cornea to flatten and the mid-peripheral cornea to thicken.9,10 A decreased density of basal cells accompanies the thinning of the central corneal epithelium, while the entire cornea experiences a reduction in keratocyte density.10
The steepening of the mid-peripheral cornea leads to myopic shift in peripheral vision and is believed to be responsible for slowing down myopia progression through reduction in axial elongation.21 However, many of the studies in orthokeratology lenses and myopia control were done on children with myopia of spherical equivalent refractive error (SER) less than −6.00 D.12,13,14
Case Study
Presentation and history
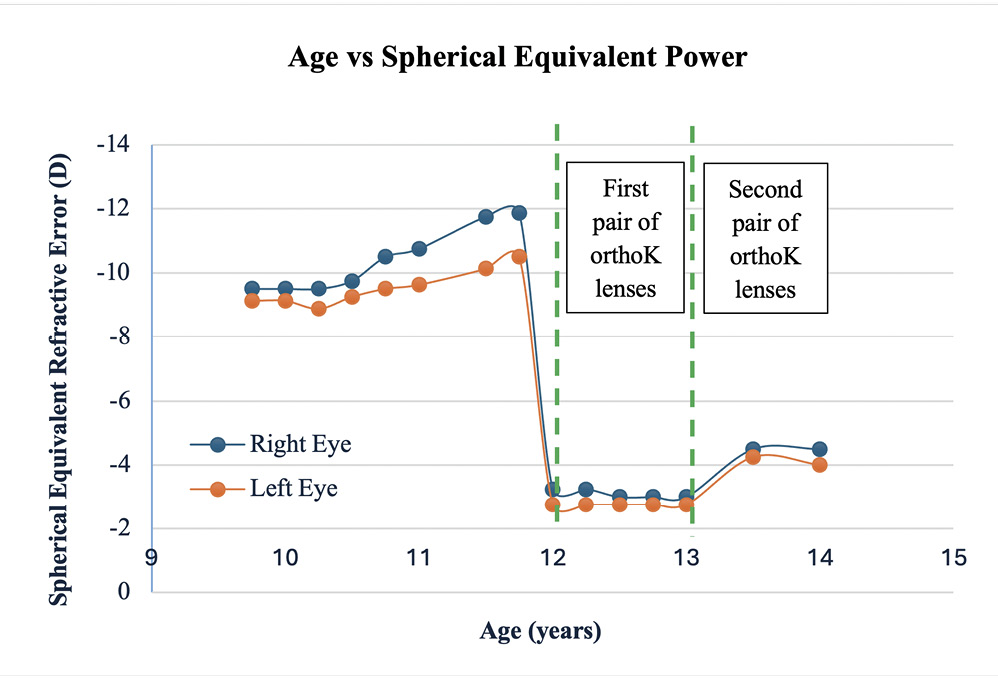
This case study provides a detailed description of a patient seen and managed at the practice of the author. The now 14-years old female patient named Naomi (pseudonym, for anonymity and compliance with data protection regulations), presented with progressive myopia and was subsequently managed with orthokeratology lenses. There was no medical or ocular history beyond myopic refractive error. She is of Chinese descent and her father had high myopia and her mother low to moderate myopia. From an early age, Naomi’s parents were concerned about her eyes, as she started wearing myopia correction (spectacle lenses) when she was six years old. Naomi’s parents were aware of the possibility of progressive myopia and controlled her visual habits strictly, limiting the hours spent on digital devices apart from schoolwork, ensured she was not undertaking additional strenuous near vision tasks. Naomi’s spectacle prescription was −11.75 D (SER) at her peak (see her full refraction details in Table 1).
Management and follow-up
Naomi first attended the practice in 2020, at the time she was almost 10 years old with SER of −9.50 D in her more myopic eye, reported to have her glasses changed (i.e. prescription updated) more frequently. Prior to attending the author’s practice, she had been fitted with blended bifocal lenses as a means of myopia control elsewhere. This treatment modality had been prescribed without regular follow-up. Upon attending and following comprehensive refractive assessment and discussion with her parents, a dual management strategy was adopted. Naomi was received a pair of progressive spectacle lenses with +2.00 D add power (Kids Myopia 1.67 with anti-reflection coating, Advance Lens Trading, Malaysia), and atropine eye drops (0.01%, 1 gtt, q. h. s.) which were prescribed and co-managed by a local ophthalmologist. Since Naomi also had intermittent exotropia of 18 PD on her right eye, she was prescribed with vision therapy. Starting from February 2020, Naomi was scheduled for close follow-up and to be re-examined every three months. However, despite the best intentions, several appointments were missed during the peak of COVID-19 pandemic. Her prolonged indoor time during the COVID-19 pandemic likely contributed to her increased level myopia, which occurred between ages ten to twelve (Table 1).4,15
Between November 2020 and April 2022 (prior to initiating orthokeratology prescription), Naomi’s myopic refractive errors had been increasing at an alarming rate, so that all management options were reviewed. A key consideration was attempting to slow down myopic progression along with axial elongation. Treatment modality options discussed were i) continuation with combination treatment of progressive lens design spectacle lenses and atropine 1%; ii) orthokeratology lenses with/or without atropine 0.01%; iii) dual-focus daily disposable myopia control soft contact lenses. Her prescription was out of range for peripheral defocus myopia control ophthalmic lenses, such as the MiYOSMART by Hoya Vision Care, since this option is limited to a maximum of combined spherical and cylindrical power of −10.00 D.
After in-depth discussion with the patient and her parents, and carefully weighing risks and benefits, a joint decision was made to fit orthokeratology lenses in April 2022, with the aim of effectively slowing myopic progression. The author chose the myOK Overnight Orthokeratology Contact Lens (Brighten Optix, Taipei City, Taiwan), because it is approved by Malaysia’s Medical Device Authority (MDA) in the author’s home country of Malaysia. This is a software-driven, advanced orthokeratology lens system. The fitting software uses each patient’s unique information to construct the initial custom order and optimize the results when modifications are necessary. The myOK orthokeratology lens (material: Boston XO2) employs an OTZ (Optimized Treatment Zone) to target myopia management in children, up to −10.00 D myopia. Similar to other orthokeratology lenses, the higher the target myopia correction, the flatter the back optic zone radius (BOZR). The author informed Naomi’s parents about the off-label use of the myOK lens due to her high myopia, which exceeds the MDA-approved range, and explained that an additional pair of spectacles would be necessary to correct residual refractive error.16,17 At this time, all parties agreed that Naomi stop using atropine eye drops at the start of orthokeratology lens wear. As per standard fitting procedure, parents were also informed on the potential risks associated with orthokeratology lenses, for example superficial corneal epithelial defects, which could render the eyes more prone to microbial keratitis.18 If the cornea were no longer susceptible to orthokeratology lenses, treatment may have to be discontinued. The importance of regular after-care visits was emphasised, and a follow-up schedule was set up (day one, three, seven and ten; then weekly, bi-weekly, monthly, and finally every three months).
Lens fitting process
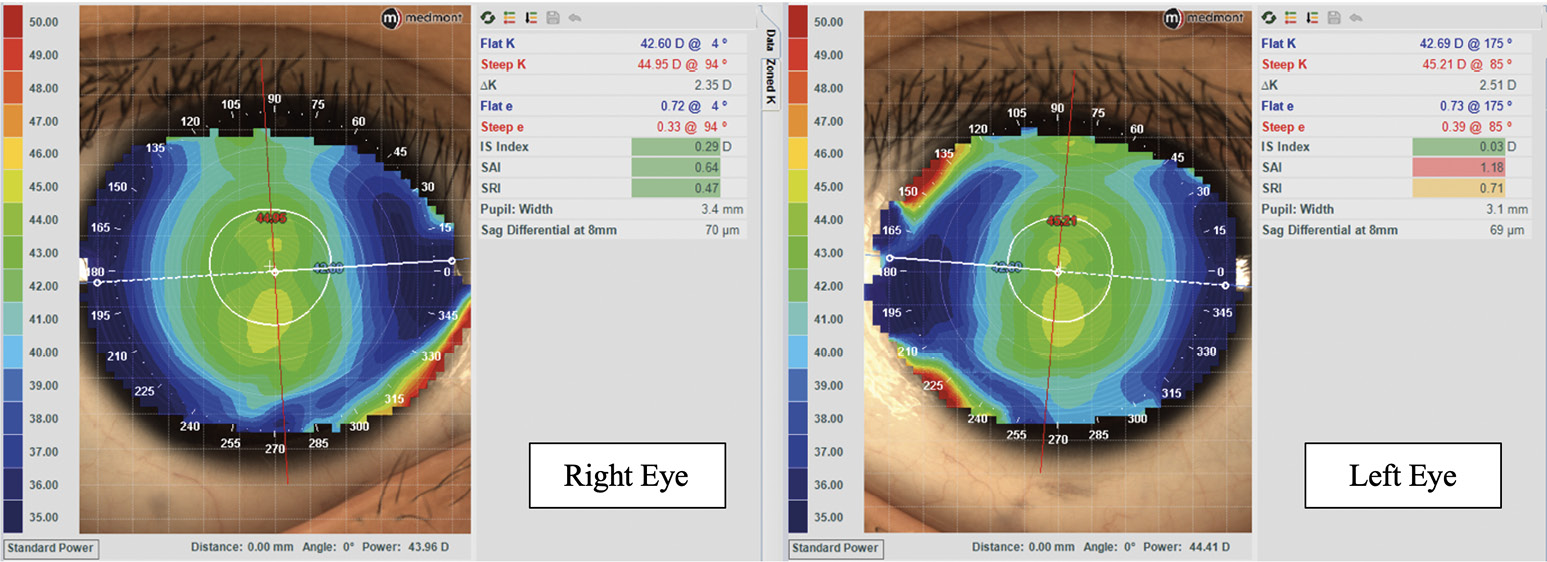
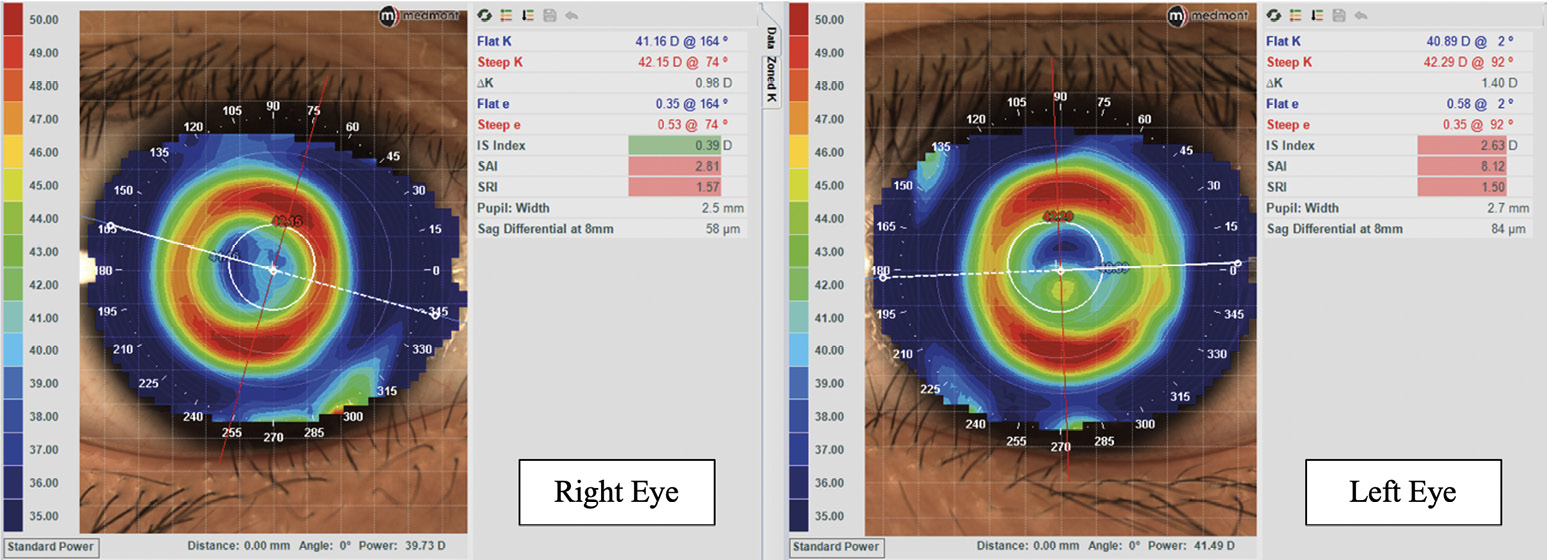
The myOK Overnight Orthokeratology, lens parameters used for Naomi are listed in Table 2. Comprehensive slit-lamp biomicroscopy of the anterior segment and corneal topography (Medmont Meridia Professional, Medmont International Pty Ltd; VIC, Australia) were carried out. All anterior structures were found to be within normal limits and negative for any signs indicating of ocular abnormality or pathology, including lids, lashes, bulbar and tarsal conjunctiva, cornea, anterior chamber, iris and pupils. Assessment of corneal topography maps revealed with-the-rule astigmatism (Figure 1); overall, her eyes were considered suitable for orthokeratology lens wear. An empirical fitting strategy was used and topography maps were sent to the manufacturer to determine the best-fit orthokeratology lens geometry, targeted with maximum target power correction for both eyes, in line with manufacturer fitting guidelines.
Patient adaptation to orthokeratology lenses and follow-up
Following receipt of the custom-designed lenses, an initial adaptation period of six weeks during which the myopic refractive error continually decreased, led to a stabilisation of the refractive status (i.e., residual refractive error and visual acuity). At this point, no refit of the orthokeratology lens was required. However, Naomi’s visual acuities were logMAR 0.63 (Snellen equivalent: 6/9) in each eye, compared to logMAR 0.00 (Snellen equivalent: 6/6) when she was using glasses.
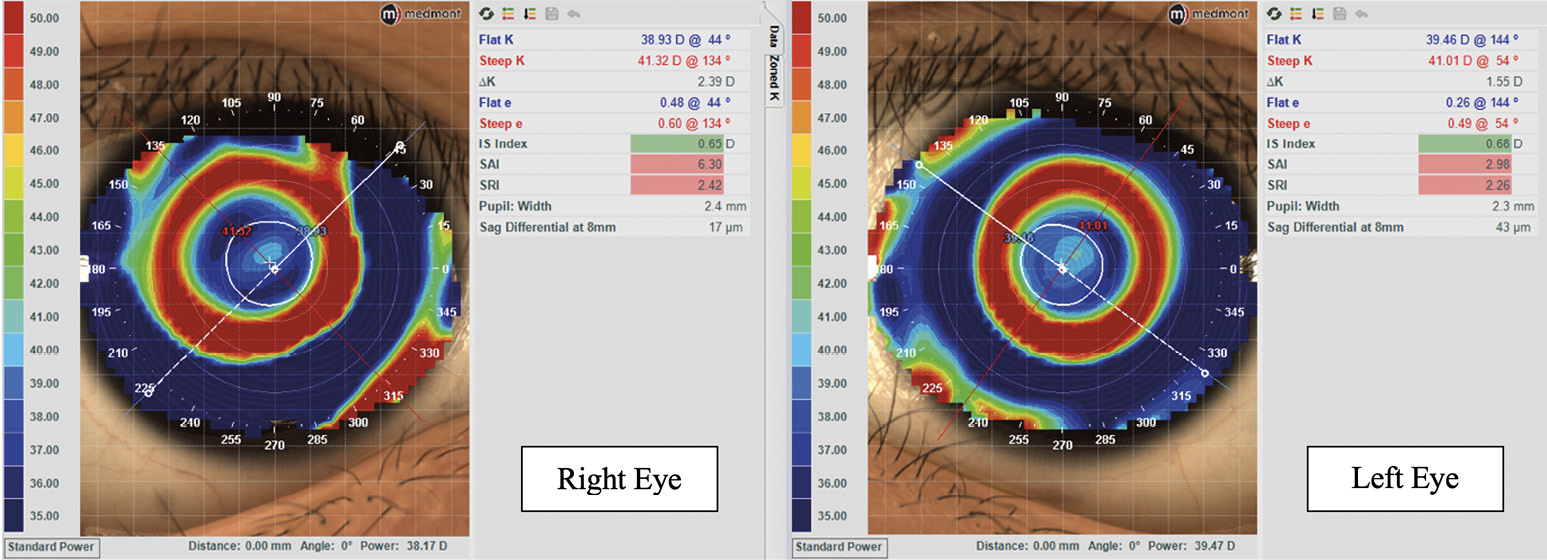
The evaluation of the lens fit revealed slight temporal decentration in both eyes (Figure 2). In orthokeratology, this decentration is common due to the temporal cornea usually being slightly steeper than the nasal cornea.8 Although previous studies have shown that smaller BOZD (< 6.0 mm) 19,20 can be more effective in myopia control, this option was not considered in Naomi’s case to not affect her visual acuities further in addition to the lateral decentration of her lenses.
An assessment of Naomi’s refractive status in May 2022 showed that her SER had decreased significantly. However, an additional spectacle correction of −3.25 D and −2.75 D was required to achieve visual acuities of logMAR 0.63 and 0.80, repectively (Table 3). Using this approach, Naomi’s SER and axial lengths remained relatively stable for 18 months, from May 2022 to November 2023. The VA achieved with orthokeratology correction was acceptable to Naomi, especially with binocular visual acuity working well for her in school. Following a year of unremarkable follow-up, an increase in myopic refractive power was noted at the age of 13 in November 2023, which corresponded to increased axial lengths (Table 3 and Figure 3). After using orthokeratology lenses, Naomi’s intermittent exotropia improved unless eyes were tired. It is well known that the use of contact lenses eliminates prismatic effect of spectacles, in myopic patients reduces exo-deviation, of the eyes, and reduced minification of retinal images, which allows for improved binocular vision and fusion.
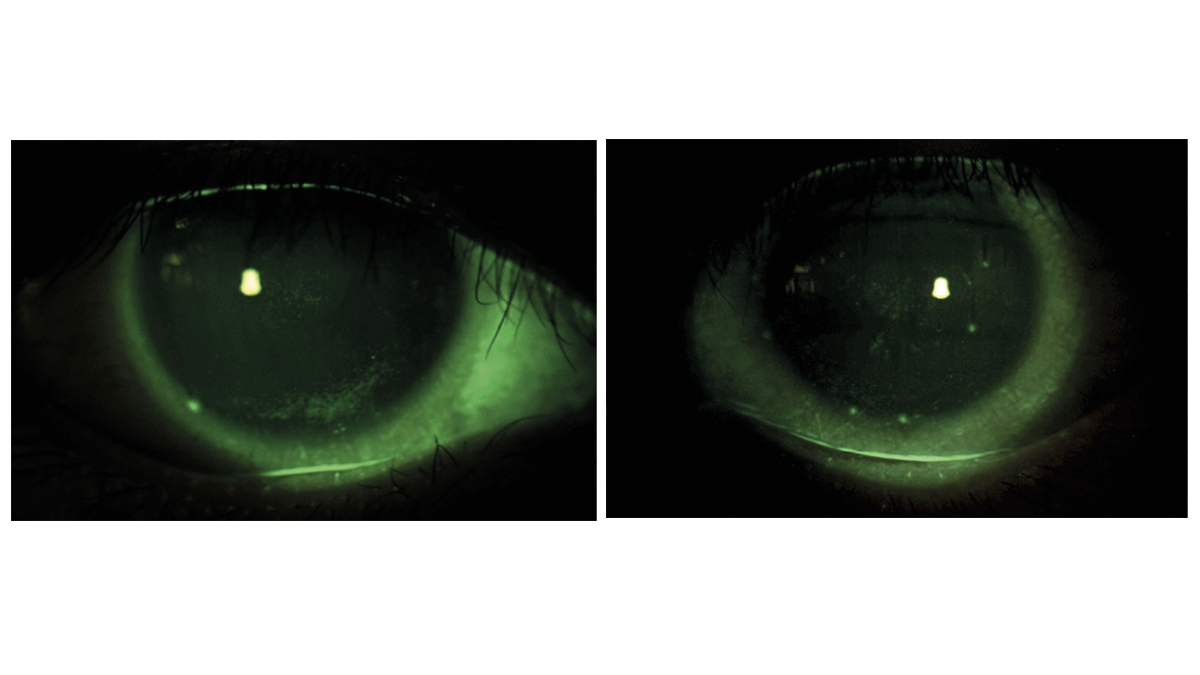
At the follow up appointment in November 2023, slight superficial epithelial corneal staining (Grade 2 to 2.5) was noted in both eyes (Figure 4), which, however, did not affect visual acuities. A slight ‘central island’ was noted in the morning on her corneal topography map, likely due to the observed corneal staining but reduced to Grade 1 in the afternoon. Naomi reported no lens biding upon waking up in the morning, except for a short period during the early stages of her orthokeratology lens wear.
With increasing academic work commitments at school, the use of more digital devices for schoolwork, Naomi reported ocular symptoms, namely a stinging sensation, as well as dryness and grittiness, especially towards the end of the day. To maintain corneal health and to reduce any risk of deterioration of the corneal staining, her orthokeratology lens parameters were reviewed and modified. Specifically, the back optic zone radius (BOZR) was changed from 10.02 mm to 9.86 mm, and 10.31 mm to 9.58 mm, on right and left eye respectively (Figure 5). Since this further reduce the refractive error correction by 1.50 D in both eyes, the additionally worn spectacles lens power was adjusted accordingly. These spectacles had powers of −4.50 DS and −4.00 DS and resulted in VA of logMAR 0.63 and 0.80, for right and left eyes respectively.
It is usually expected that orthokeratology lens wear, when used to correct high myopia, carries a higher risk of cornea staining.18 Currently, Naomi uses a medium viscosity conditioning eye drop (Acuaiss Ultra – Preservative Free, DISOP, Spain) to moisturise contact lenses and the ocular surface prior to lens insertion. A more viscous conditioning eye drop may have the potential to further reduce the severity of corneal staining but could also cause more lateral decentration of the lenses. She was prescribed with hydrogen peroxide disinfecting solution, either Hidro Health H202 (Disop, Spain) or Aosept Plus (Alcon, USA) with sodium chloride sterile saline as rinsing solution. To ensure compliance, corneal health is under continuous regular monitoring.
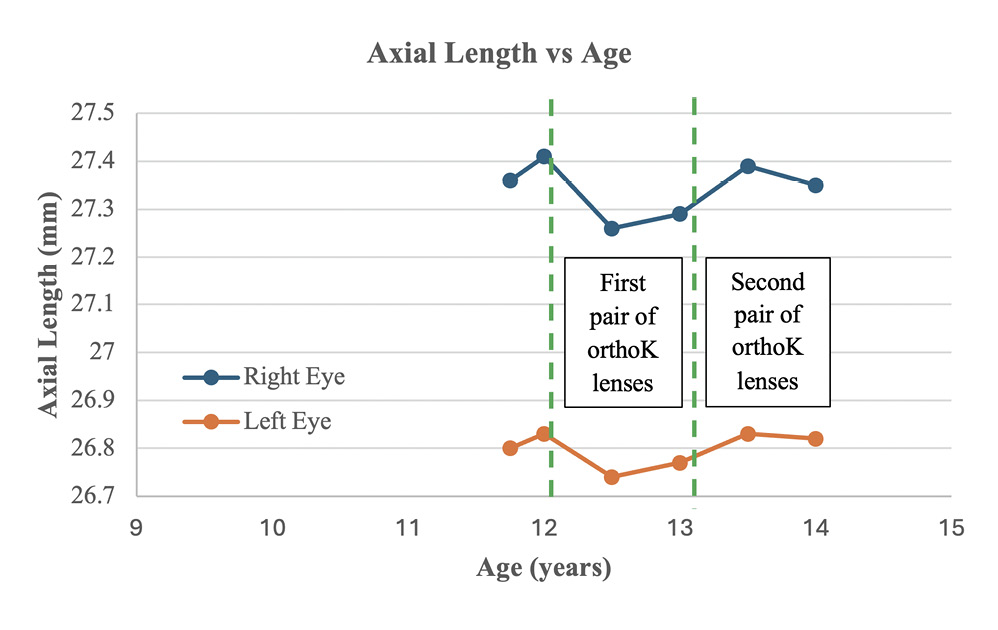
Since orthokeratology correction is aimed at slowing down myopic progression, axial elongation is a key ocular parameter to monitor treatment efficacy.21 In addition, orthokeratology was historically primarily used to correct myopia, with its benefit for slowing the progression of myopia becoming obvious substantially later.4,14,21 For Naomi, early baseline axial length measurements were unavailable due to unavailability of an ocular biometer at the author’s practice prior to March 2022. Following the initial orthokeratology lens use, there was slight reduction in her axial length of 0.15 mm and 0.09 mm on right and left eyes respectively. Over the two year period, Naomi’s axial lengths remained relatively stable, compared to pre-orthokeratology lens wear (Figure 6). In addition to the change in her residual refractive errors after using her second pair of orthokeratology lens with slightly steeper BOZR, axial lengths had slightly increased in both eyes. Overall, Naomi’s relatively stable axial length is considered a promising sign in myopia management that is aligned with findings of previous studies by using this treatment modality.15,16,17,21
Conclusion
This case study details the use of orthokeratology lenses in a young patient with high myopia. Overall, the treatment is considered successful because it has drastically reduced the measurable myopic refractive error as intended. Even though a substantial residual refractive error remained, the patient and her parents were content with the treatment result and open to consider the use of a pair of additional spectacles.
Ultimately, it is important to balance treatment decisions between efficacy of the chosen myopia control strategy, satisfactory visual acuity, corneal health and slowing down of axial length elongation. The patient’s commitment to lens wear, continuous practice of good hygiene, discipline and parents’ understanding and commitment, are pre-requisites for successful orthokeratology lens wear. The case described represents the highest degree of myopic refractive error that has been managed at the author’s practice to date. However, there are further highly myopic patients who are currently being managed with orthokeratology lens modalities, all without or just minimal complications such as low grade superficial corneal epithelial staining.
A possible limitation of this case study is the duration of the patient’s orthokeratology lens wear period of two years and the patient’s age.11 Early cessation of orthokeratology lens wear is not recommended unless compliance issues occurred, and that myopia has to be monitored regularly every three to six months, to prevent a rebound effect.22 Myopia management could be continued up to late teenage years (i.e., 18 years old) or when axial elongation slows, and myopia stabilised, yet definitive guidelines are not available.23,24
Acknowledgements
The author would like to thank Sven Jonuscheit for his continuous support and feedback in the write up of this case study.
Conflict of interest
The author declares that there is no conflict of interest.
Logan, N. S., Naidoo, K., Resnikoff, S., Sankaridurg, P., Smith III, E. L.,
Troilo, D. and Wildsoet, C. (2019) IMI- Myopia Control Reports Overview and Introduction. Invest. Ophthalmol. Vis. Sci., 60, M1-M19
for axial elongation in Asian children. Ophthalmic Physiol. Opt., 43,
1160-1168.
