Periocular basal cell carcinoma
Purpose. Basal cell carcinoma is the most common malignant tumor in the periocular area. It typically presents as a painless and slow growing nodule, however, the appearance can vary. It is associated with UV exposure and is more common in fair skinned individuals. The aim of this article is to highlight a case of periocular basal cell carcinoma and to discuss the diagnosis and appropriate treatment options.
Material and Methods. A Caucasian patient presented with a round, non -resolving lesion medial to left medial canthus. Incisional biopsy of the lesion revealed a basal cell carcinoma. The patient was properly educated on the diagnosis and treatment options.
Results. The lesion was successfully treated with a full thickness excision followed by eyelid reconstruction. It is crucial to be aware of all potential treatment options.
Conclusion. This case discusses the diagnosis and management of periocular basal cell carcinoma. Optometrists can play a key role in diagnosing and co-managing eyelid malignancies.
Introduction
Basal cell carcinoma is the most common malignant tumor in the periocular area.1 It typically presents as a small painless and pearly raised nodule and most often affects the medial lower eyelid. Central ulceration may occur with associated bleeding.2 Fair-skinned individuals are at greatest risk and those with a history of sun exposure. Hereditary factors are also involved in the development of basal cell carcinoma.3
Case presentation
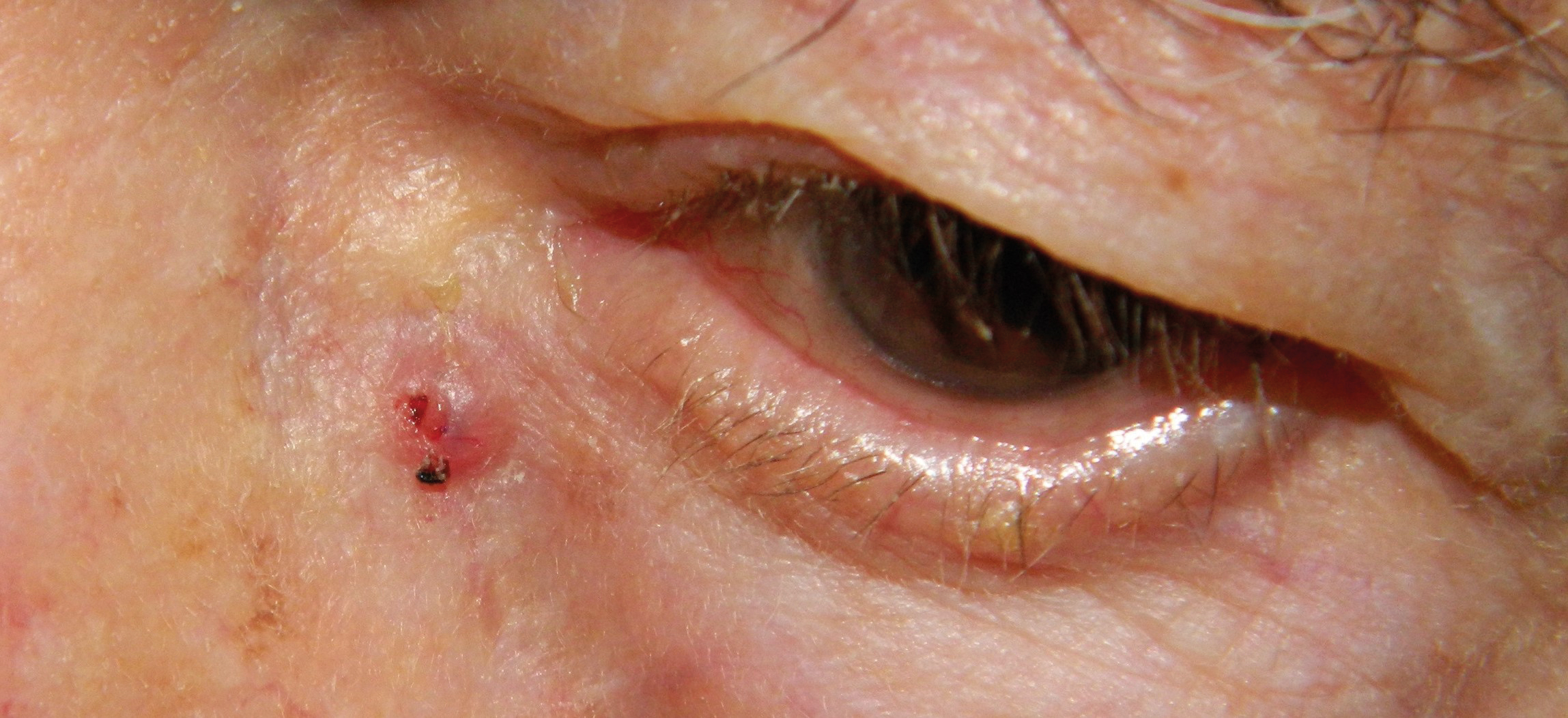
A 92-year-old fair skinned male with a history of multiple skin cancer excisions was referred to the eye clinic from dermatology for a suspicious lesion on their left medial canthus. Patient notes that they previously had a basal cell carcinoma on his face and underwent Mohs micrographic surgery. This treatment involves repeatedly removing and microscopically evaluating thin slices of tissue from a lesion and its surrounding area until no cancer cells are detected. Their past skin cancer history includes a squamous cell carcinoma on the dorsal surface of his right hand and a basal cell carcinoma adjacent to their left side of the nose near their left nostril for which they also had Mohs micrographic surgery. Addition medical history includes hypertension, hyperlipidemia, ulcerative colitis, rheumatoid arthritis, and aortic stenosis. Medications included adalimumab, nifedipine, atorvastatin, a low dose aspirin, and calcium. Ocular history was positive for bilateral cataract extraction ten years prior. The exam findings are as follows: uncorrected distance visual acuity was: 20/30 OD, 20/40 OS. Pupils were equal, round, reactive with no APD. Extraocular motilities were full and confrontational visual fields were full in each eye. Slit lamp exam revealed meibomian gland dysfunction and telangiectatic vessels along the eyelid margins. A round, pearly, elevated, erythematous lesion was noted medially to the inferior nasal canthus. The lesion measured 0.5 × 0.5 cm and had a small area of ulceration (Figure 1). The conjunctiva, cornea and iris were unremarkable OU. IOP was 12 mmHg in both eyes. A dilated fundus examination revealed well centered multifocal intraocular lenses OU, healthy optic nerve heads with 0.3 cupping OD and 0.25 OS. Maculae and peripheral retinae were within normal limits. The retinal vasculature revealed mild arteriolar attenuation. The patient was educated on the periocular lesion and potential differentials. It was decided to perform an incisional biopsy of the lid lesion. The pathology results revealed basal cell carcinoma, nodular type. The patient was educated on the biopsy results and potential treatment options. The patient returned 2 weeks later, and the lesion was removed by full thickness excision by Mohs surgery (Figure 2) followed by reconstruction by our oculoplastic surgeon.

Discussion
Basal cell carcinoma (BCC) is the most common periocular skin cancer. It represents about 90 % of the malignant eyelid tumors especially in fair skinned individuals with a history of sun exposure of which the periocular region is a highly sun exposed area.3 These carcinomas, as the name suggests, involve the basal cells of the epidermis that begin to replicate uncontrollably.4 Higher risk populations for BCC include older patients with fair skin and a history of sun exposure. This might include those who work outside like landscapers or gardeners with unprotected skin. In general, it is associated with the cumulative sun exposure over years and it is why older patients are diagnosed more often.5 BCC has various clinical subtypes, but no universally accepted histological classification exists. However, nodular, and superficial subtypes of BCC tend to be the least aggressive forms while micronodular, morpheaform, and infiltrative subtypes are all less common but represent a higher risk for being more invasive, have a higher recurrence rate, and higher risk for metastasis. In fact, these three subtypes represent 80 % of BCC associated with orbital invasion.6 The anatomical location of most BCC includes most commonly the lower lid, followed by the medial canthus and then the upper lid.2 Nodular BCC more commonly looks pearly with overlying vessels and may have central ulceration. The superficial subtype may have a reddish coloration with a scaly surface in addition to the pearly borders. Ulceration may also be present on the anterior surface of any of the more aggressive subtypes. Sometimes other characteristics such as indistinct borders or multiple nodules may be helpful in suggesting a more aggressive subtype such as morpheaform or micronodular.7 Ultimately, it is a pathological diagnosis.
The differential diagnosis of BCC can include benign lesions as well as other carcinomas. For instance, benign lesions might include chalazion, sebaceous cysts or hyperplasia, or actinic keratosis. Other carcinomatous differentials might include melanoma, which would appear more pigmented, squamous cell carcinoma (SCC), sebaceous cell carcinoma, or Merkel-cell carcinoma. All these carcinomas are more aggressive, characterized by more rapid growth, and have much higher rates of metastasis.8 In general, helpful examination tips in differentiating between benign and malignant lesions include anatomical change in the area of and surrounding the lesion, change in skin coloration or inconsistent coloration within the lesion or the adjacent area. At the eyelid margin itself, associated lash loss can be highly predictive of a carcinomatous lesion.9 Finally, examining the palpebral conjunctiva including lid eversion can assist in evaluating potential deeper invasion. Artificial intelligence (AI) is an emerging tool for helping to detect periocular BCC. Deep learning is used to identify benign versus malignant periocular lesions. A 2022 study conducted in China, tried to develop a deep learning system using digital photographic images using ordinary digital cameras. This was called an eyelid tumor detection system (ETDS). It used 1,533 eyelid tumor images (1,161 benign and 372 malignant tumors) as the learning set.10 The system ultimately had a sensitivity equivalent to an expert examiner, but it scored lower in specificity of malignant tumor detection. It outperformed both junior and senior level ophthalmologists. AI systems may be on the way to assist in screening for periocular BCC and other malignant lesions.
Biopsy is the gold standard for diagnosing BCC. Surgical excision is the most common treatment option which may include micrographic surgery (Mohs). In this technique tissue within the lesion is removed as well as tissue at the margins of lesion with pathology evaluation to ensure that the margins are clear of carcinomatous cells. Mohs is designed to minimize tissue damage to offer the best cosmetic outcome for the patient.11 Non-surgical options include topical immunotherapy such as imiquimod (IMQ). IMQ is an immunomodulator that causes apoptosis of the tumor cells. It is a 5 % cream that is dosed once per day five times per week for 8 - 16 weeks.12 This treatment is more often offered for the small nodular subtype of BCC when surgery is not possible. The potential side effects may include foreign body sensation, conjunctivitis, blurred vision, keratitis and lacrimation. Typically, these resolve after treatment is concluded. Another topical option is 5 % 5- fluorouracil (5-FU) cream, an antimetabolite, can be used for both small BCC and SCC. However, IMQ was found to have better efficacy.13 In addition, radiotherapy can be offered as an adjunctive treatment for patients with aggressive BCC with perineural invasion or for those patients who cannot undergo surgical excision. Side effects may include secondary cataracts, dry eye, ectropion, radiation retinopathy and optic neuropathy.2 Finally, oral therapy includes Vismodegib. This is a class of medication called a hedgehog pathway inhibitor. This pathway plays a key role in cell growth in BCC cancer. The drug blocks the G protein-coupled receptor smoothened, which suppresses the BCC. Therapy is offered as adjuvant therapy for advanced disease that is not amenable to surgery as well as metastatic disease. It’s dosed at 150 mg per day. Side effects may include things like weight loss, muscle spasms, alopecia, and decreased appetite.14 It is important to note that Vismodegib is contraindicated in pregnancy because it may cause severe harm to the developing fetus.
Conclusion
Basal cell carcinoma is the most common tumor of the malignant tumor of the periocular area. Although it is certainly less aggressive than other periocular malignancies, early detection is a key predictor of better outcomes. As eye doctors it is critical to be on the lookout for BCC in our patients with high-risk demographics: Caucasian, older age, light complexion with personal history of significant sun exposure, and personal or family history of BCC or other skin cancers. One should be on the lookout for typical characteristics of BCC including pearly lesion borders with vascularization, ulceration, irregularity of lesion borders that appear scaly, hyperemic or discolored, Also, associated lash loss at the lid margin is a key indicator or of a potential malignant lesion. In addition, everting lids in suspicious areas can assist in determining potential depth of invasion. AI systems may become an additional tool in assisting the detection of malignant lesions in the periocular area. The gold standard is biopsy, but clinical examination guides the necessity for biopsy. Although micrographic surgery is the gold standard for treating BCC, non-surgical options may include topical IMQ and 5 F-U for smaller less aggressive subtypes. Radiotherapy and oral Vismodegib can be considered as adjunctive treatment for non-surgical candidates and those with recurrent or metastatic spread.
Conflict of Interests:
The authors declare that there is no conflict of interests regarding the methods and devices mentioned in the article.
Carcinomas. Curr. Health Sci. J., 46, 167-172.
Nelemans, P. J., Kelleners-Smeets, N. W. J. (2018). Five-Year Results of a Randomized Controlled Trial Comparing Effectiveness of Photodynamic Therapy, Topical Imiquimod, and Topical 5-Fluorouracil in Patients with Superficial Basal Cell Carcinoma. J. Invest. Dermatol., 138, 527-533.
