Practice case: Correctly assessing disease risks
Purpose: A comprehensive optometric eye examination in a patient is described. Medical history and results of standard screenings tests lead to further selection of required measurements.
Material and Methods: The following optometric measurement methods were used: measurement of visual acuity (bon Multivisus®), refraction, contrast sensitivity test (Vistech-chart Type A), Amsler grid, slit lamp examination (slit lamp bon SL-85) with evaluation of the anterior and posterior eye (Volk 78 D Lens), Easyscan (a confocal Laser-Scanning-Ophthalmoscope), measurement of intraocular pressure (Non-contact Tonometer Reichert AT555) and perimetry (Zeiss Humphreys Perimeter).
Results: Visual acuity, especially at near vision, was significantly improved with a new prescription and lens type. Several risk factors for glaucoma were identified. The appearance of the optic nerve head, perimetry results and Amsler grid appearance were also suspicious. Therefore, the patient was referred to an ophthalmologist.
Conclusions: History and simple screening tests can give indications in every refraction to the presence of eye conditions and provide more information for more specific testing. In the present case, an intraocular pressure measurement without additional tests would have led to an incorrect result in the estimation of the risk of glaucoma. Therefore, intraocular pressure measurements should not be performed without additional tests.
Introduction
For optometric eye examinations, the guidelines of the German professional association “Zentralverband der Augenoptiker und Optometristen (ZVA)” do not specify a rigorous measurement/testing procedure. At each examination, the basic screening tests should be supplemented by additional tests and examination procedures depending on the results. Mandatory are history, motility, cover test, pupil reaction, visual acuity, refraction and binocular vision testing. If there are deviations from the expected values, these measurements can be extended anterior and posterior eye examination, color vision test, contrast sensitivity test, twilight vision test, perimetry, tonometry, topography, pachymetry or other tests.1 While eye examinations by ophthalmic opticians and optometrists in Germany are primarily performed in the context of determining visual acuity and refraction for the prescription of glasses or contact lenses, optometrists in the UK are seen as primary eye care providers and are also expected to detect eye diseases. The “Principles of the routine eye examination” state, that an optometrist besides the sight test “must perform an internal and external examination and carry out such additional examinations as appear to be necessary to detect signs of injury, disease or abnormality in the eye or elsewhere”.2,3 Therefore, in addition to vision tests for monocular and binocular refraction and a slit lamp, the mandatory optometric equipment in the UK always includes a tonometer and a perimeter.4 Thus the scope of practice of British Optometrists differs to some extent from that of German optometrists. In the UK the optometrist is mainly the primary eye care provider and may also work in the treatment of some eye diseases.5
Screening
Screening should be performed for diseases, which can be diagnosed and treated in an early stage. Typical examples of screening tests in optometry are diabetic retinopathy, age related macular degeneration and glaucoma.6
Glaucoma
According to the guidelines of the professional and scientific associations “Berufsverband der Augenärzte” (BVA) and the “Deutsche Ophthalmologische Gesellschaft” (DOG) glaucoma screening includes taking a medical history with determination of risk factor evaluation, funduscopy with analysis of the optic nerve head and the retinal nerve fiber layer, a tonometry (ideally applanation tonometry) and a slit lamp examination of the anterior eye. If glaucoma is suspected, perimetry should also be performed. . If normal pressure glaucoma is suspected, a daily intraocular pressure profile can be done to assess the diurnal pressure variations. The patient can also be referred to a specialist in internal medicine. When glaucoma is diagnosed, therapy usually consists of lowering the intraocular pressure with glaucoma eyedrops.7 8 Some studies suggest, that lowering the intraocular pressure is not always successful in halting the progression of glaucoma. In case of disturbed retinal perfusion pressure due to a high venous pressure, an additional therapeutic management may be the use of antioxidants.9 This therapy can be an option, if no central venous pulse is seen in the optic nerve head, which may be a sign of a disturbed retinal perfusion pressure.10
Age related macular degeneration
BVA and DOG recommend in their guidelines to examine the macula from the age of 55 years. In addition to ophthalmoscopy, medical history taking, assessment of metamorphopsias and visual acuity are obligatory. If AMD is suspected, additional measurements such as OCT or fluoresceine angiography are indicated.11
Diabetic retinopathy
Patients with diabetes should be regularly examined for eye diseases as part of their disease management program. Examination methods include medical history, visual acuity and slit lamp examination of the anterior and posterior eye. Patients with abnormalities can be referred to the general practitioner or a diabetologist.12
Case study
A 69-year-old patient visited the private optometric practice for an optometric eye examination, because his near and distance vision had deteriorated. The following screening test/examination procedure was flexible and oriented to the results of patient’s medical history and results of basic screening tests, such as Amsler grid.
Methods
The tests/examinations were performed according the guidelines “Arbeits- und Qualitätsrichtlinien für Augenoptik und Optometrie” (work- and quality guidelines for ophthalmic optics and optometry).1 All measurementes were performed by the same optometrist.
Medical History
The patient was asked about the reason for his visit and about his vision problems. A history of eye diseases, general health, medication and family was also taken.
Visual acuity
Visual acuity with the patient’s own glasses was measured with line letters on the bon Multivisus (bon optic, Lübeck, Germany).
Refraction
The refraction was performed with the cross cylinder examination in a trial frame. Binocular vision status was tested with the D6-test.
Contrast sensitivity
The contrast sensitivity was quantified monocularly with the Vistec chart type A with normal room illumination. If a grid direction was designated as incorrect, the last correctly recognised pattern was recorded as the measured value.
Amsler Grid Test
A white on black Amsler grid was used in a distance of 40 cm and the visual function was tested separately for the right and left eye. The patient was asked to look at the white dot in the center of the grid and fixate it constantly. The patient was then asked to name or show areas of distortion.
Slit lamp examination of the anterior and the posterior eye
The slit lamp examination was performed with a bon SL-85 slit lamp (bon optic, Lübeck, Germany). The eyelids, tearfilm, conjunctiva, cornea, anterior chamber angle and lens were examined. The anterior chamber angle was estimated with van-Hericks method. Thereby a narrow slit beam with an illumination angle of 60° is projected on the temporal limbus. When the slit is moved nasally the distance between the band of light on the cornea and on the iris is estimated on the point where the iris is first illuminated. Optic nerve head, macula, blood vessels and the fundus of both eyes, as far as visible without dilation, were examined on the slit lamp with indirect ophthalmoscopy and a Volk lens 78D (Volk Optical Inc., Mentor, Ohio, USA). The optic nerve head was assessed with respects to the CDR, ISNT-rule, local atrophy of the neuroretinal rim, course of the blood vessels and possible haemorrhage. Analysis of the macula contained the assessment of drusen, pigmentary changes, haemorrhages, exudates and other anomalies. In addition a fundus photo for documentation was taken with the Easyscan (EasyScan B.V., Rijswijk, the Netherlands), which is a confocal laser-scanning-ophthalmoscope.
Intraocular pressure
The measurement of the intraocular pressure was performed at 12.00 noon with a non-contact tonometer Reichert AT555 (Reichert Inc., Depew, New York, USA). The average of the values was calculated.
Visual fields
For visual field measurement the Sita 24-2 strategy of a Zeiss Humphreys perimeter (Carl Zeiss Meditec, Oberkochen, Germany) was applied. For each visual field measurement one eye was covered with an eye patch.
Results
Medical History
In addition to his distance and near vision problems, the patient stated that he had a history of hyposphagma. Hypertension was known and is treated with medication. Only antihypertensives are taken regularly. Family history includes a known history of glaucoma on the paternal side. Last visit to an optometric practice was two years ago in the UK.
Visual acuity
Lens power of the existing, two-year-old varifocals and visual acuity with these glasses:
R sph -3.75 cyl -2.75 A 67° Add +2.5 VA 0.5
L sph -3.50 cyl -2.25 A 115° Add +2.5 VA 0.63
Refraction
Results of refraction and visual acuity
R sph -3.25 cyl -3.25 A 80° Add +2.5 VA 0.8
L sph -3.75 cyl -2.25 A 115° Add +2.5 VA 0.8
Contrast sensitivity
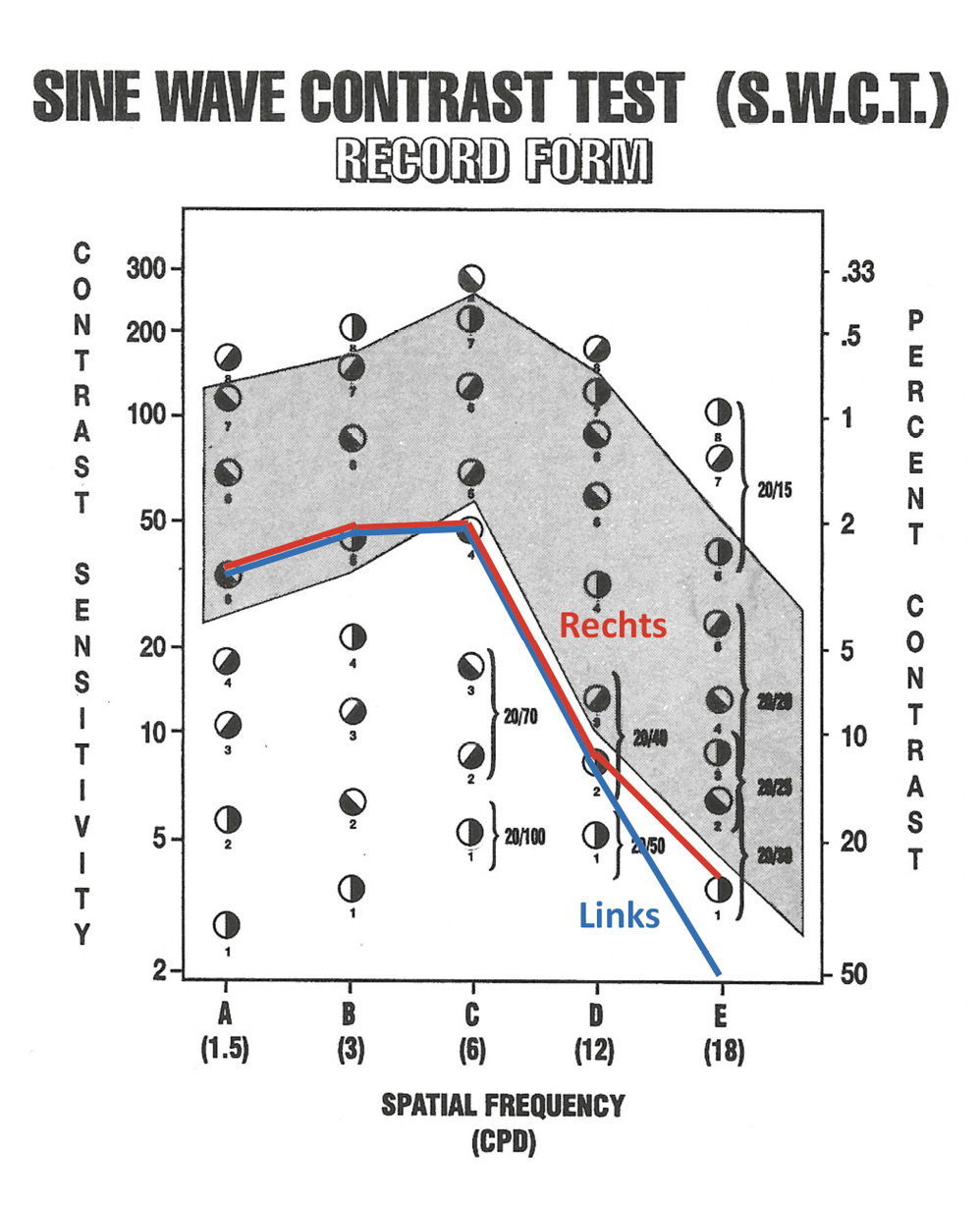
Figure 1 shows the patients contrast sensitivity curve on the Vistec chart. Results in the grey area of the chart are achieved by 90 % of all people between 10 and 70 years of age. The test result is outside normal limits if the contrast sensitivity in the spatial frequencies A to C is at least 2 rows below normative data.6 In the present case, the contrast sensitivity curve is in the lower range of normative data.
Amsler Grid
The right eye showed distorsions in the centre and to the left of the central fixation target. In the left eye the patient described general distorsions over the whole grid. This test result lead to a thorough macular examination on the slit lamp of both eyes in the further examination.13
Slit lamp and anterior eye examination
The examination of the tear film (tear film meniscus 0.2mm, BUT 12 s), the eyelids, the conjunctiva (CCLRU Grade 2) and the cornea (no punctuate infiltrates, no scars) revealed no abnormalities OU. Due to the maximum VA of 0.8 the cristalline lens was examined for opacities. Beginning opacities of the posterior cortex were documented. The anterior chamber angle was open (van Herick Grade 4). This is equivalent to an angle of 35 – 45 degrees.14 As the patient is myopic this is in line with the expected result.15
Slit lamp examination of the posterior eye and fundus scan
Figure 2 and 3 show the fundus of the right and the left eye. Both images were taken with the Easyscan Confocal Laser-Scanning-Ophthalmoscope.
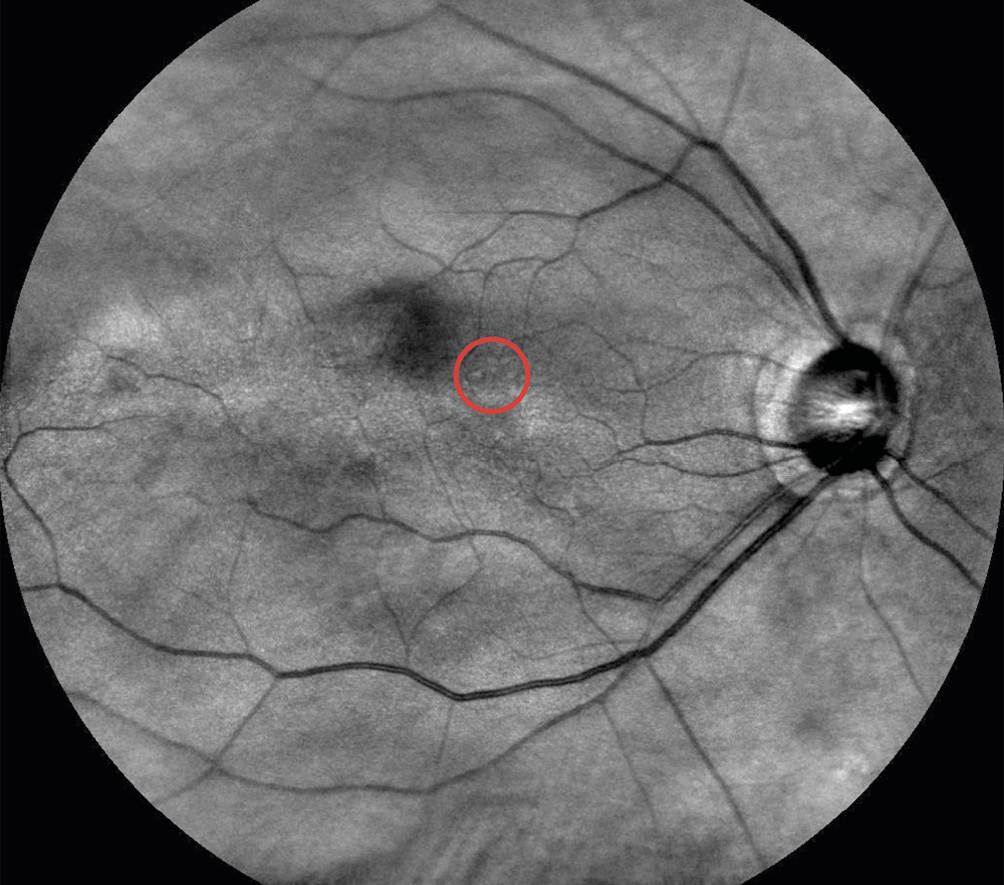
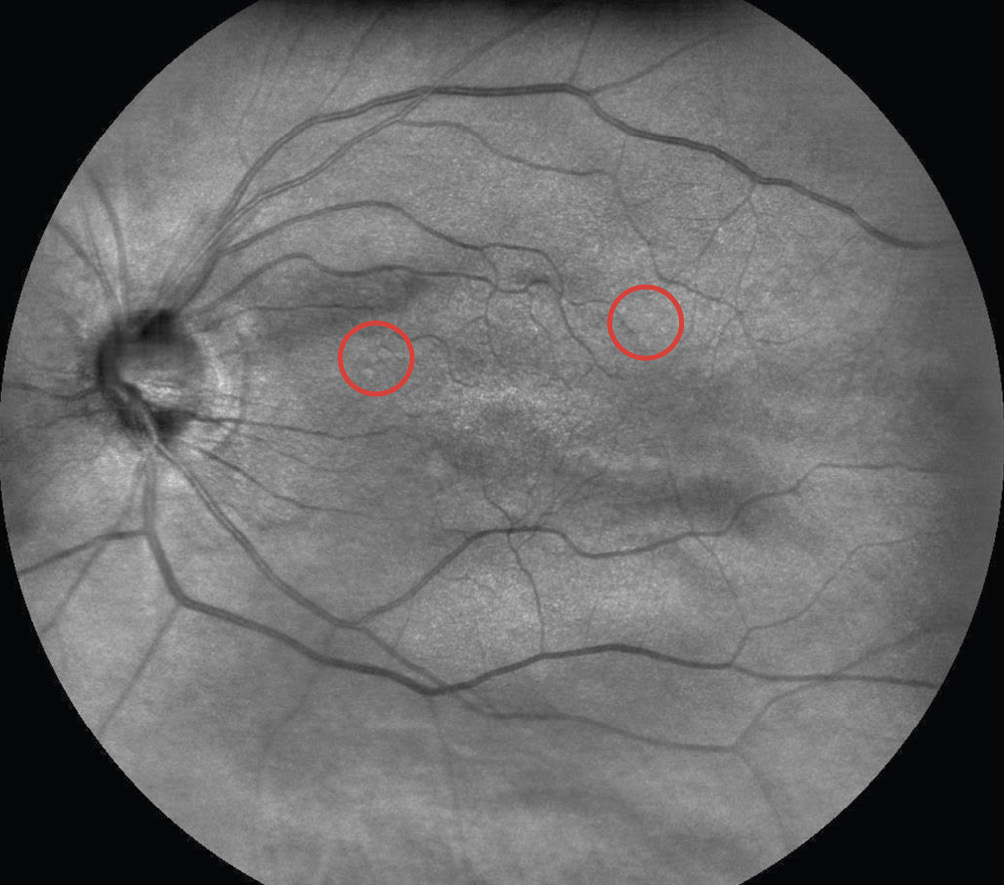
Macula
Few mid-sized drusen were present in the enlarged macular area of the right eye and outside the macular area of the left eye. Due to the distorsions the Amsler grid, the macular area was examined for further anomalies such as epiretinal gliosis and macular edema.16 Direct fundus examination of the retina did not conform this. Therefore, further measurements were indicated.
Blood vessels
The ratio of arteries and veins was 2:3 and thus normal. Typical clinical signs of a pathologic hypertensive retinopathy were not present.
Optic nerve head
The cup disc ratio assessed on retinal photography was 0.6 OU.17 A value of more than 0.5 for the CDR is considered suspicious. The appearance of the optic nerve head OD was consistent with the ISNT rule. Blood vessels were located nasally. The neuroretinal rim of the optic nerve head OS was significantly thinner inferiorly than superiorly (not consistent with the ISNT rule). In addition the optic nerve head OS showed a tilted disc.
Intraocular pressure measurement
The average of the IOP of three measurements at 12 noon was 13.7 mmHG OD and 17.0 mmHg OS.
Visual field measurement
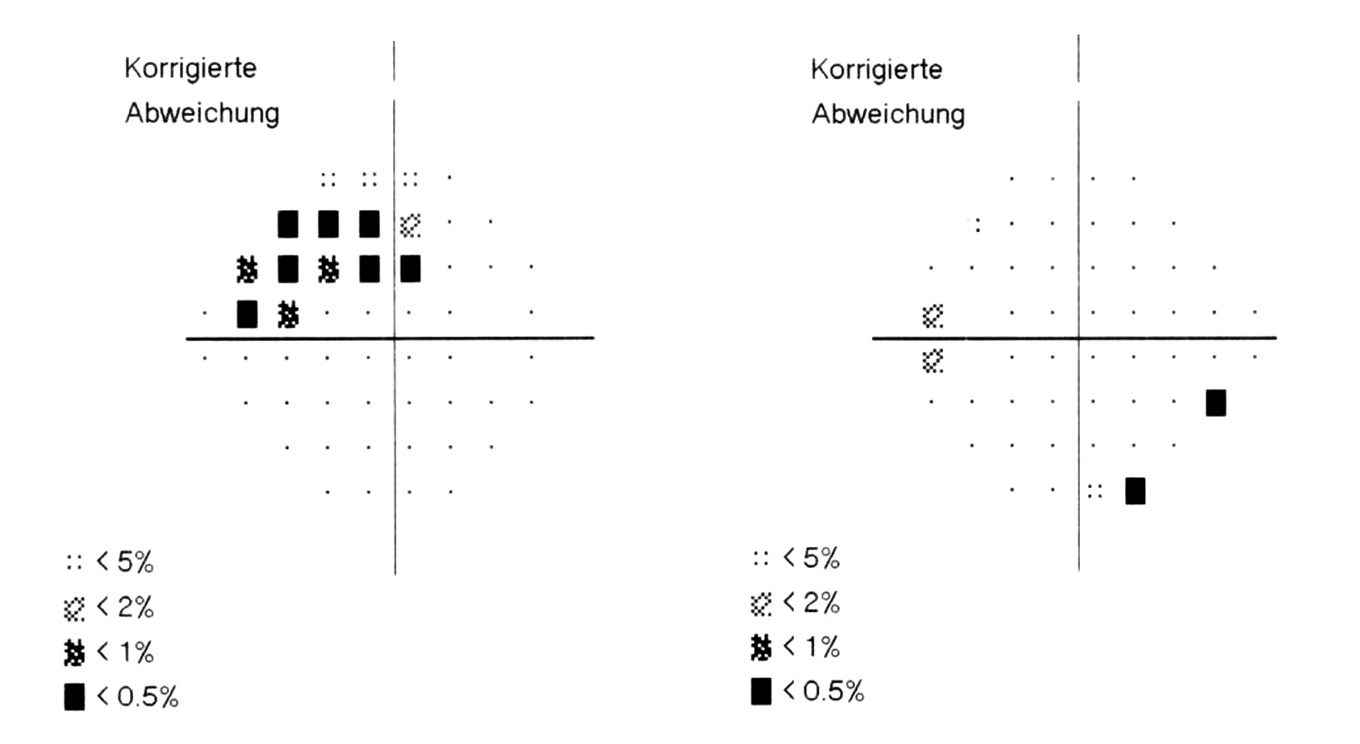
The pattern deviations of the visual field measurements of both eyes are shown in Figure 4. In the right eye an arcuate relative visual field defect superior can be seen. On the left eye only individual points in the visual field were statistically outside normal limits. The glaucoma hemifield test of the left eye was graded as “borderline”.
Discussion
Glaucoma
The medical history already revealed some risks for POAG. These are:
- Positive family history in the parent generation Risk: 2x
- Myopia of at least 4D Risk: 2 -3x
- Age above 60 years Glaucoma prevalence: 1,4%
According to the DOG rules, annual control of glaucoma and other age-related retinal changes is recommended even in the presence of a risk factor in patients over 60 years of age.18 Therefore, an examination of the anterior chamber angle, the optic nerve head, IOP and visual field test were performed. The anterior chamber angle was quantified on the slit lamp with the van-Herick technique. This method is less accurate than gonioscopy or Scheimpflug imaging, particularly in differentiating between degrees of anterior chamber angle, but is adequate and highly repeatable for general classification as open, narrow or closed anterior chamber angle.19 In the present case only a general assessment of an open or closed anterior chamber angle with risk for narrow angle glaucoma was required. The result of a van Herick Grade 4 was realistic as myopic eyes are less likely to have narrow angles as compared to hyperopic eyes.15 The intraocular pressure was below 21 mmHg. However, it cannot be rule out, that due to significant fluctuations of the IOP, the intraocular pressure is above the threshold at a different time of the day. Therefore neither intraocular pressure above the threshold range nor normal tension glaucoma can be excluded.20 Glaucoma is more common when there is a greater difference in IOP between the two eyes. Regarding to a study by Williams et al. the probability of having glaucoma is 6 % when the difference of the IOP between the right and the left eye is 3 mmHg. The risk of glaucoma increases with increasing IOP asymmetry. With an IOP difference of 6 mmHg the likelihood for glaucoma is 38 %.21 In the case of a possible normal tension glaucoma, Flammer's syndrome should be considered, which can lead to glaucoma due to circulatory disorders. The Flammer syndrome is more common in women, thin people and people with office jobs. It is indicated by cold extremities, low blood pressure and decreased thirst and pain-sensation.22 When normal tension glaucoma is suspected, patients should be interviewed for these symptoms. In the present case, such an in interview was not carried out.
On the left eye glaucoma-typical changes of the optic nerve head were the excavation, a vertical CDR of 0.6 and the neuroretinal rim, which did not comply with the ISNT rule. The visual field of the right eye showed a glaucoma-typical pattern. Judging from this result one would expect, that the neuroretinal rim on the right eye was against the ISNT rule. However, it is possible that due to the tilted disc ISNT rule was not correctly assessed.23 For a better assessment of the CDR, the size of the optic nerve head should have been measured. In large optic nerve heads - large cup disc ratios of 0.6 and even more can be statistically normal (within the 95th percentile), whereas in smaller optic nerve heads cup disc ratios of more than 0.5 are statistically outside normal limits. A general measurement of optic disc size could improve the assessment of the CDRs.24 A measurement of the central corneal thickness could have improved the assessment of the IOP, as measured IOP in thin corneae is lower than the actual IOP.25 A normal-tension glaucoma is defined as a type of glaucoma with an IOP below 21 mmHg, typical papilla excavation and visual field defects.26 This patient had a Bjerrum-scotoma in the right eye and a glaucoma typical excavation of the optic nerve head in the left eye. Even if only one criteria applies to each eye, the patient should be referred to an ophthalmologist in a timely manner.
Age related macular degeneration
A thorough analysis of macular changes is required due to the distorsions on the Amsler grid. Metamorphopsia may be observed when photoreceptors are delocated, e.g. when fluid is underneath the macular retinal tissue. The most common cause for metamorphopsia is macular edema, which can occur in wet AMD or diabetic retinopathy for example. Dry AMD with drusen and epiretinal membranes rarely leads to distorsions on the Amsler grid.16 The fundus of both eyes showed some drusen. Signs of an epiretinal membrane or exudates were not found, but cannot be excluded with slit lamp and SLO fundus examination only. Smaller exudates can better be diagnosed with other methods like fluorescein angyography or OCT.27 It is likely that the drusen present were not perceiveable on Amsler grid and are not the cause of the perceived distorsions. Without further measurements like optical coherence technology (OCT) the causes of the metamophopsias cannot be clarified. Therefore, the patient was referred to an ophthalmologist for further evaluation.
Hypertensive Retinopathy
The patient was treated with medication for high blood pressure. In the past, he suffered from a hyposphagm. If hyposphagms occur repeatedly it may be a sign of suboptimal medication, atherosclerosis or systemic anticoagulants.28,29 However, the blood vessels on the retina do not show typical hypertensive signs.30 Therefore, the patient was told to see his GP if the hyposphagm reoccurs.
Cataract
Contrast sensitivity was within normal limits but in the lower range of the normal curve. In addition, at the maximum VA of 0.8 OD and OS, optical media, especially the crystalline lens, were examined. Some opacities in the posterior cortex were visible in the crystalline lens some opacities were visible in the posterior cortex. However, this did not lead to subjective impairments. According to the definition of the DOG cataract is a lens opacity with an impact on visual abilities, especially visual acuity.31 As the patient was consulting us for the first time, no comparison of VA to former results was possible. Subjectively, the patient had no visual problems with the new prescription.
Evaluation of the results
Distance and near vision was improved with the new glasses. For near vision, changing the lens type to an office lens resulted in a significant subjective improvement. In addition, the patient was advised to use a bright lighting when reading due to the beginning opacities in the crystal lens. Furthermore, a timely visit to an ophthalmologist was recommended, especially due to the distortions on the Amsler grid and the suspicion for glaucoma.
Diagnosis
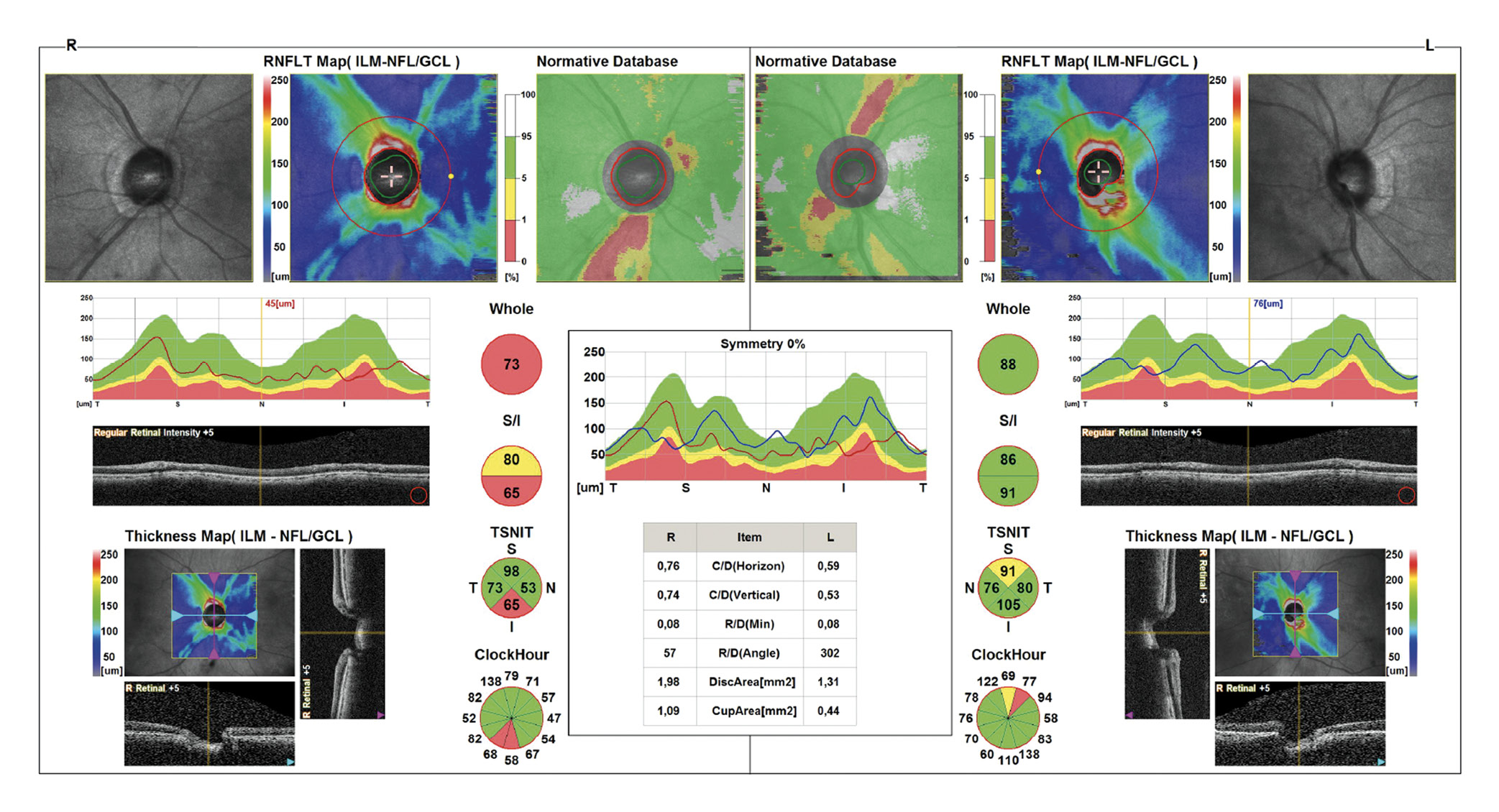
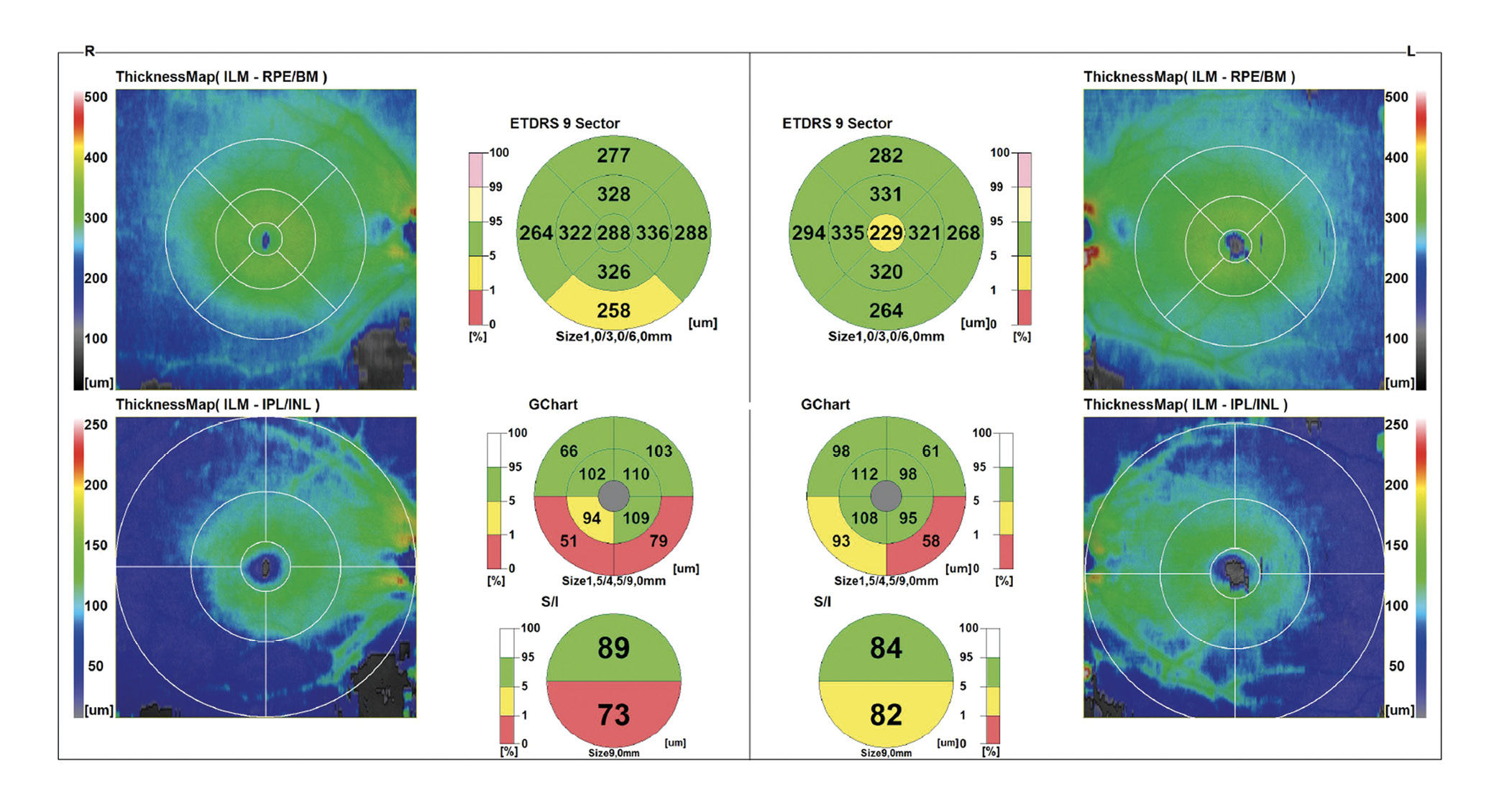
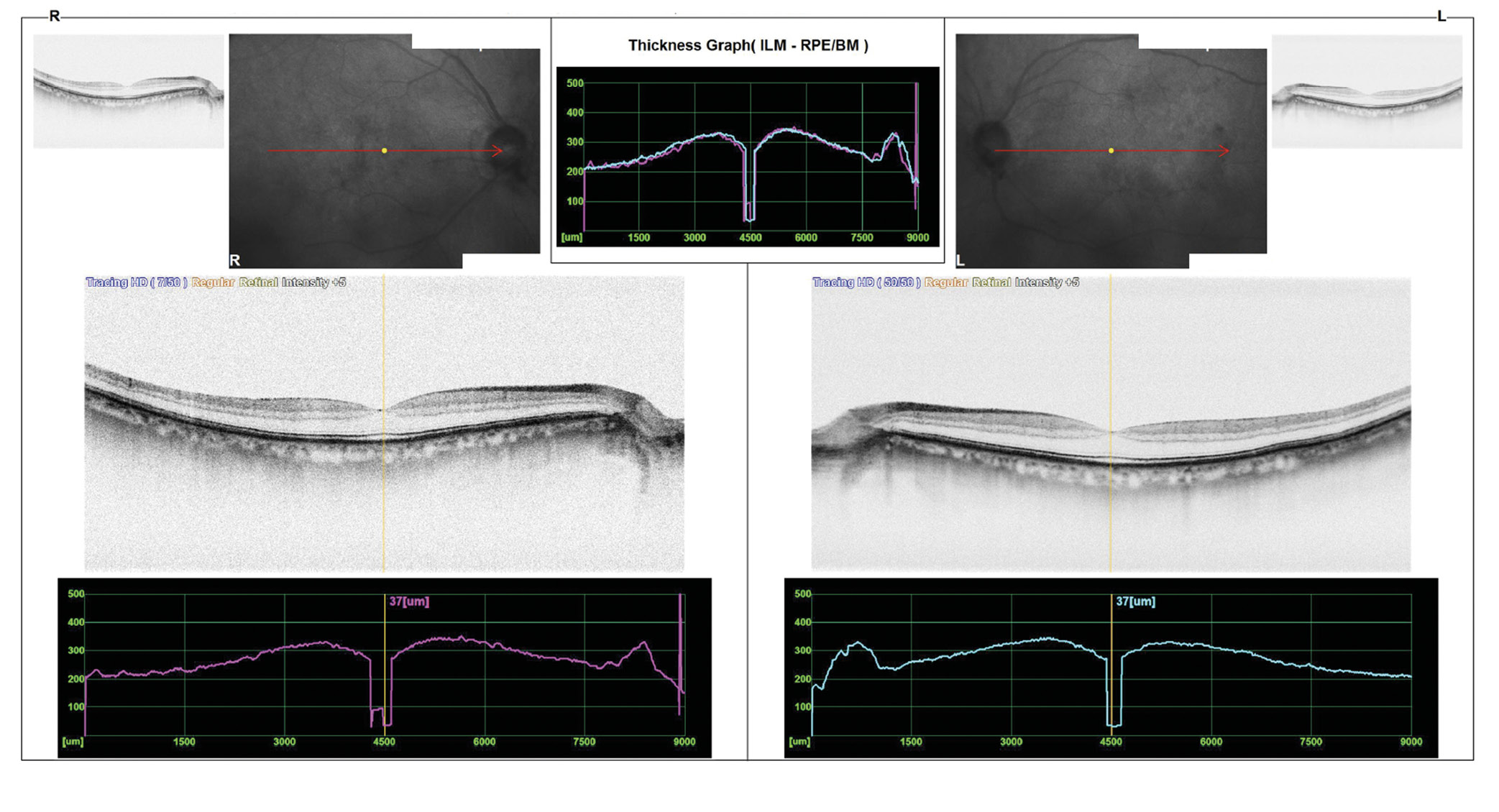
The patient visited the ophthalmologist a few weeks later and was diagnosed with glaucoma, which is treated with glaucoma eye drops. OCT images of the optic nerve head including a measurement of the nerve fiber layer (Figure 5), the ganglion cell layer in the macular area (Figure 6) and a macular OCT image (Figure 7) OU were taken. The appearance of the macula was normal (Figure 7). The ganglion cell layer in the right eye was significantly thinner (Figure 6). The inferior neuroretinal rim was also significantly thinner in the right eye (Figure 5). This corresponds to the visual field defect observed. On the OCT image, the CDR OD was specified 0.8. The automatic segmentation estimated a very large cup. As only these printouts of the OCT images were available, it could not be clarified whether the automatic segmentation of the OCT was correct. Therefore, original data are required for a thorough interpretation of OCT images. Some retinal rim changes were also present in the left eye, but these were less significant. In addition, the automatic segmentation on the left optic nerve head inferior was not correct, limiting the assessment of the optic nerve head.
Conclusion
In the present case, the patient visited the practice for new glasses in order to get better vision for near and distance. According to the ZVA guidelines, a medical history and general screening tests/examinations are required in addition to the refractive measurements. The patient’s history revealed an increased risk for glaucoma. Amsler grid results also were outside normal limits. In cases of deviations from the norm and abnormalities during the refraction procedure, the ZVA guidelines recommend further testing, without specifying which test should be performed depending on the previous results. Due to the risk of glaucoma, additional tests/examinations such as IOP measurement, visual fields, examination of the posterior eye and anterior chamber angle measurement were performed. Only two of these four tests had results outside normal limits - visual field testing and the optic nerve head appearance.
This case shows that, if possible, all relevant tests and measurements should be performed during an eye examination and not just a selection of them.
Conflict of interest
The author declares that there is no conflict of interests regarding the methods and devices mentioned in the article.
