Scleral lens fitting after paediatric limbal dermoid removal
Purpose. This case report describes the management of refractive error and amblyopia using a scleral lens fitted to the eye of a young child with an irregular cornea resulting from limbal dermoid removal and corneal transplant in infancy.
Material and Methods. A young infant was initially fitted with spectacles and occlusion therapy following the surgical excision of a limbal dermoid and full thickness corneal transplant. The vision did not improve in spite of patching so the child was referred for contact lens fitting. Various iterations of scleral lens fitting were carried out.
Results. Scleral lens fitting was attempted from the age of 2 years but transplant rejections, the COVID-19 pandemic and variable cooperation meant that adequate lens wear could not be achieved in the early stages. In addition, the corneal shape changed during the course of the fitting. During these periods, spectacle wear and occlusion therapy were maintained until a good lens fit could be achieved following several modifications. Treatment is ongoing but at the age of 5 years, the visual acuity is 0.24 logMAR letters.
Conclusion. Scleral lenses can be used to habilitate the vision in an eye with an irregular cornea but when scleral lens wear is not possible, it is important to persevere with spectacle correction and patching therapy. Several iterations of scleral lenses may be needed as the eye changes and the child grows.
Introduction
A corneal dermoid is a choristoma, a mass of normal tissue found in an abnormal location. It is characteristically a mass of dermis or skin type tissue, covered with keratinised and possibly hairy squamous epithelium. Dermoids can be singular or multiple and can involve the full-thickness of the cornea.1 They can be isolated or can be associated with a systemic disorder such as Goldenhar syndrome.
Treatment may be carried out on cosmetic grounds or in an attempt to improve the visual outcome. Surgical options include resecting the lesion to a level plane, or by carrying out a lamellar or full thickness keratectomy using donor tissue in order to maintain corneal and scleral integrity.1 An alternative treatment is deep lamellar excision followed by sutureless multilayered amniotic membrane transplantation.2
High hypermetropia and astigmatism are the most common refractive errors in patients with limbal dermoids undergoing lamellar keratoscleroplasty.3,4 Worse visual outcomes are more likely in children with larger dermoids, requiring larger grafts.5
Amblyopia is common in children with dermoids and needs to be managed carefully with occlusion therapy from a young age. The aim of fitting a contact lens to an eye that has undergone lamellar keratoplasty is to produce a regular corneal surface that can give the best chance of a good visual outcome.
Contact lenses, especially rigid lenses have been used for the rehabilitation of irregular corneas for a very long time with scleral lenses first being fitted for irregular keratoconic corneas by Adolf Fick in Germany in 1888.6 Corneal lenses can be used to mask small amounts of corneal irregularity but where the irregularity is marked, corneal lenses tend to be unstable. A larger scleral lens then becomes a better option and where necessary, numerous types of modification can be made to improve the lens fit.7 Various other types of corneal irregularity and opacification can also benefit from being fitted with scleral lenses, including post-keratoplasty, corneal scarring, refractive surgery and corneal dystrophies. In a retrospective review of children under 13 years who were fitted with scleral lenses after the failure of conventional therapy, the majority were fitted for corneal surface disease with only 13 % of patients fitted for refractive disorders.8

Materials and methods
A 7-week old infant initially presented at Moorfields Eye Hospital in January 2019 with a diagnosis of a limbal corneal dermoid cyst involving the inferotemporal cornea of the left eye, and left secondary astigmatism. There was no significant ocular or family history and there were no other lumps such as pre-auricular dermoids. The infant was visually alert and did not show a particular preference for the right eye. Cycloplegic refraction showed mild hypermetropia, appropriate for age, and left astigmatism.. The hypermetropic prescription increased in the left eye over the next few months and at the age of 6 months, glasses were prescribed with the prescription in the left eye of +9.00 / −2.00 x 90.
At the age of 9 months, a surgical excision of the limbal dermoid was carried out with an 8 mm anterior lamellar
keratoplasty. The sutures were removed just over 2 months later and the patient was discharged with Dexamethasone drops followed by ongoing once daily Fluorometholone 0.1%.
At the age of 1 year, vision was recorded as OD 0.50 (Cardiff Cards) and OS fixing and following. Further refraction was carried out and the glasses prescription was changed to: OD Plano OS +10.00 / −4.00 x 130.
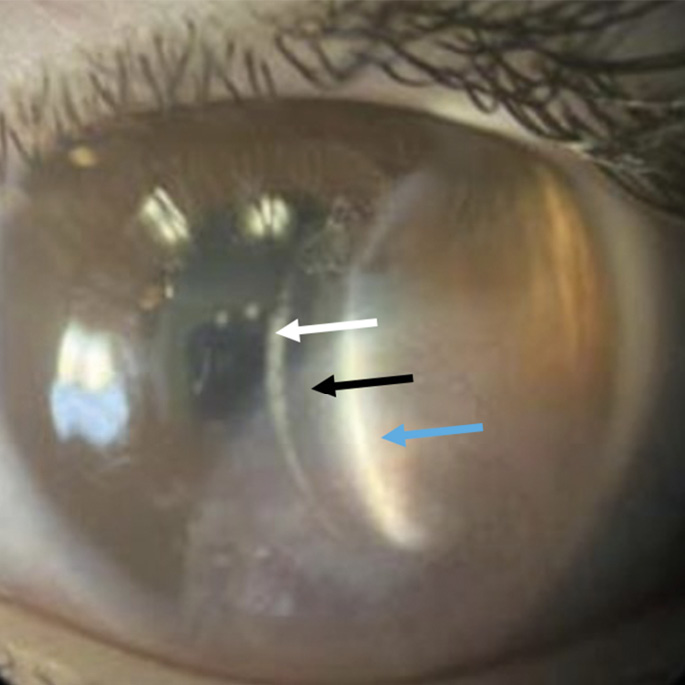
Patching was commenced for 4 hours/day to the right eye and the infant was referred for a contact lens trial. The aim was to reduce the anisometropia and to provide better visual correction to the irregular surface of the eye. Figure 1 shows the appearance of the eye with a clear corneal graft at that stage. Unfortunately, the fitting appointment was cancelled due to the COVID-19 pandemic and the child was next brought to Accident & Emergency four months later with a red eye. Examination revealed an epithelial rejection line on the surface of the corneal graft. This was treated with Dexamethasone drops which reversed the rejection.
Contact lens fitting
Six months later, vision was found to be OD 0.10 OS 1.20 Kay logMAR Singles with glasses. Contact lens fitting was attempted with a Bausch & Lomb Zenlens Z9 scleral which centred well but there was a large mobile bubble and touch over the graft area. The clearance was 300 microns centrally but no clearance over the grafted area of the cornea and limbus. An increased clearance (sag) lens was ordered therefore and it was decided that because of the difficulty inserting a non-fenestrated lens in such a young child, the lens should be ordered with fenestrations for ease of insertion
and removal.
The following lens was ordered: Zenlens (Bausch & Lomb) Z9 7:80:17.00: +6.25DS Sag 5150 microns with increased limbal clearance zone of 200 microns and 1 fenestration 3 mm from the edge of the lens.
The lens was inserted but the bubble created from the fenestration was partially obscuring the visual axis so a further two evenly spaced fenestrations were added 4 mm from the edge of the lens in an attempt to break up the larger bubble. This was successful and the lens was issued in April 2021 with advice to build up the wearing time slowly to 5 – 6 hours and a telephone follow up appointment was arranged two weeks later. At that appointment, the parent reported that the child’s cooperation with lens insertion was poor so lens wear was abandoned for the time being and they continued wearing glasses and patching for four hours a day.

In May 2021, the patient again attended Accident & Emergency following a two day history of the left eye being red. A sub-stromal haemorrhage was noted with a 2 × 3 mm graft infiltrate at the graft border. The anterior chamber was well-formed and no leak was noted. Polymerase Chain Reaction (PCR) samples were taken to test for bacteria, fungus and other microbes and 2-hourly Moxifloxacin drops were started in the left eye.
Two days later, the corneal graft was surgically debrided from the host cornea due to the worsening microbial keratitis and large corneal graft ulcer. Pathology testing was carried out on the specimen and Moraxella Nonliquefaciens was found. The patient was discharged on Monofloxacin 0.5% four times a day and Natamycin 5% hourly.
The eye settled well but by July 2021, spectacle vision had deteriorated to 1.20 @ 1 m with Kay logMAR pictures, possibly in part because they had not done any patching for several weeks. A new spectacle prescription was ordered OD Plano, OS +10.00 / −2.50 x 145 and the parents were encouraged to resume patching for four to six hours a day to the right eye. At a subsequent appointment, the vision had improved to 1.30 Kay logMAR pictures.
Contact lens wear remained suspended on the advice of the child’s consultant ophthalmologist and it was not until the eye had been quiet and comfortable for nearly a year that in May 2022 a further contact lens appointment was made. By then, the co-operation was something of an issue so the parents were advised to practice holding the child’s eyelids apart with washed hands. Once that was achieved, they were asked to buy some ocular lubricants (preservative free) to instil on a daily basis so the child would once again get used to something going into the eye. A new 17 mm Zenlens scleral was ordered, with the same specifications as before, but without fenestrations as the ocular surface profile had changed post-graft excision and it was felt that this would be better for the ocular surface.
When the child returned to try this lens two months later, it appeared that the excised graft area was more prominent than before (Figure 2). There was concern that the 17 mm diameter lens might cut across the thin excised area and cause problems so a larger diameter scleral lens was trialled (18 mm) with a an open limbus to give more clearance over the dermoid. An Innovative Scleral trial lens OH7 8.22:18.00 / −0.25 sag 5560 µm fitted reasonably but there was an area of touch over the dermoid. A lens with an increased sag was therefore ordered: Innovative Scleral OH9 7.58:18.00 / +1.50DS with a sag of 5880 µm. The child’s cooperation was very good at this visit and it was possible to insert the lens air-free.
Results
By the time this lens was issued, the child was four years old. The lens was found to fit well and was non-fenestrated with no bubbles (Figure 3). There was good to adequate clearance, no touch over the treated area and no significant blanching. The parents were advised to slowly build up the wearing time at home and also continue patching the fellow eye 3 – 4 hours/day.
The child was not keen on wearing the lens much during the next year but they continued with glasses, patching and intermittent lens wear. Regular lens wear was commenced in November 2023, together with ongoing patching for three to four hours a day, and the now 5-year old attended the clinic two months later wearing the lens. The visual acuity was measured as 0.24 logMAR letters. The lens was fitting well although there was some ingress of bubbles into the superior pre-corneal tear reservoir.
Bubbles under the lens is an ongoing problem but this has been reduced by inserting the lens using a slightly viscous solution of preservative-free carmellose sodium 1%. When the patient next returns for follow up, we will consider reducing the sag of the lens if necessary.
Discussion
The removal of a limbal dermoid in infancy is likely to result in corneal astigmatism and an irregular cornea. Dense amblyopia will ensue if visual habilitation is not started early. A scleral lens will provide a stable fitting in such an eye and needs to be worn in conjunction with occlusion therapy.
When fitting young children with non-fenestrated scleral lenses, compliance is essential since a lens cannot be inserted and removed on a daily basis without the child being amenable. The patient discussed here was unfortunate because during the period when contact lens fitting was being undertaken, there were two episodes of transplant rejection requiring treatment and appointments had to be cancelled or postponed due to the COVID-19 pandemic. This resulted in the child being more reluctant to have the contact lens inserted afterwards and so it took some time before compliance was sufficient to attempt contact lens wear. Severinsky & Lenhart 9 described a similar patient where lens wear was abandoned after an episode of graft rejection. In the patient discussed in this case report, lens fitting was again attempted after the eye had been quiet for nearly a year.
During the whole period, occlusion therapy was maintained using a sticky patch. Atropine penalisation was not considered due to the risk of reverse amblyopia 10 since the amblyopia in the affected eye was considered to be dense and the infant was very young. It has been found that preoperative treatment of amblyopia can improve postoperative visual acuity 11 so it was hoped that continuing with the occlusion therapy whilst wearing spectacles, would improve the final acuity with the contact lens. This did indeed prove to be the case.
Conclusion
This case report discusses the early years’ path taken by an infant born with a limbal dermoid who managed to achieve a good visual outcome. In conditions with a high degree of corneal irregularity, rigid lenses are needed to improve vision and a scleral lens is the most likely option that will provide a stable and comfortable fitting. In a young patient, optical penalisation needs to be initiated and continued throughout the amblyogenic period in conjunction with spectacle and/or contact lens wear for there to be any hope of achieving and maintaining reasonable acuity.
Acknowledgements
The authors would like to thank Mr Ken Pullum for his advice in fitting this patient and also thank Professor Frank Larkin for Figure 1
Conflict of interest
The authors declare that there are no conflicts of interest regarding the methods and devices mentioned in the article.
209-15.
Q., 24, 25-31.
