Scleral Lens Management in a Patient with Ectasia and Diplopia
Purpose: The present case report describes a patient with post-Lasik ectasia and vertical binocular diplopia seeking to regain clear and single vision.
Material and Methods: This was achieved through prescribing scleral lenses with prism and utilizing high Dk material (tisilfocon A) to address the prism induced increased lens thickness.
Results: The clinical outcome was favorable with the patient enjoying all day lens wear without compromised corneal health while maintaining single and clear vision.
Conclusion: The case report demonstrates that scleral lenses with a vertical prismatic effect can also be successfully fitted to treat vertical diplopia.
Introduction
Ectasia is a common indication for scleral lenses, but a less common indication is the treatment of heterotropia through prism. The uniquely stable design of scleral lenses allows for incorporation of prism in any direction, including horizontal.1 The present case report describes a scleral lens prescribed with prism achieving clear and single vision in a patient with irregular astigmatism and diplopia from a vertical heterotropia.
Case Description
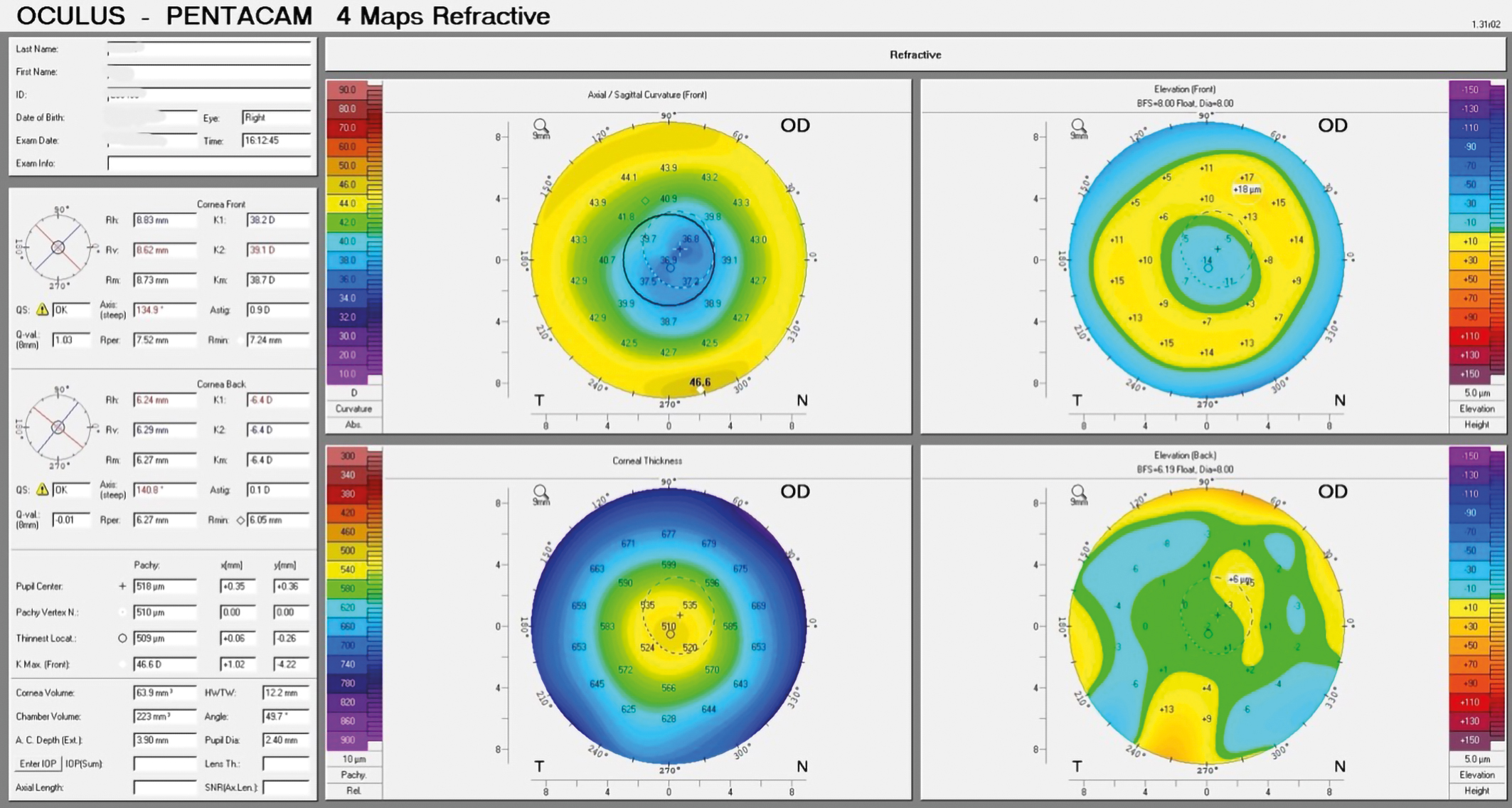
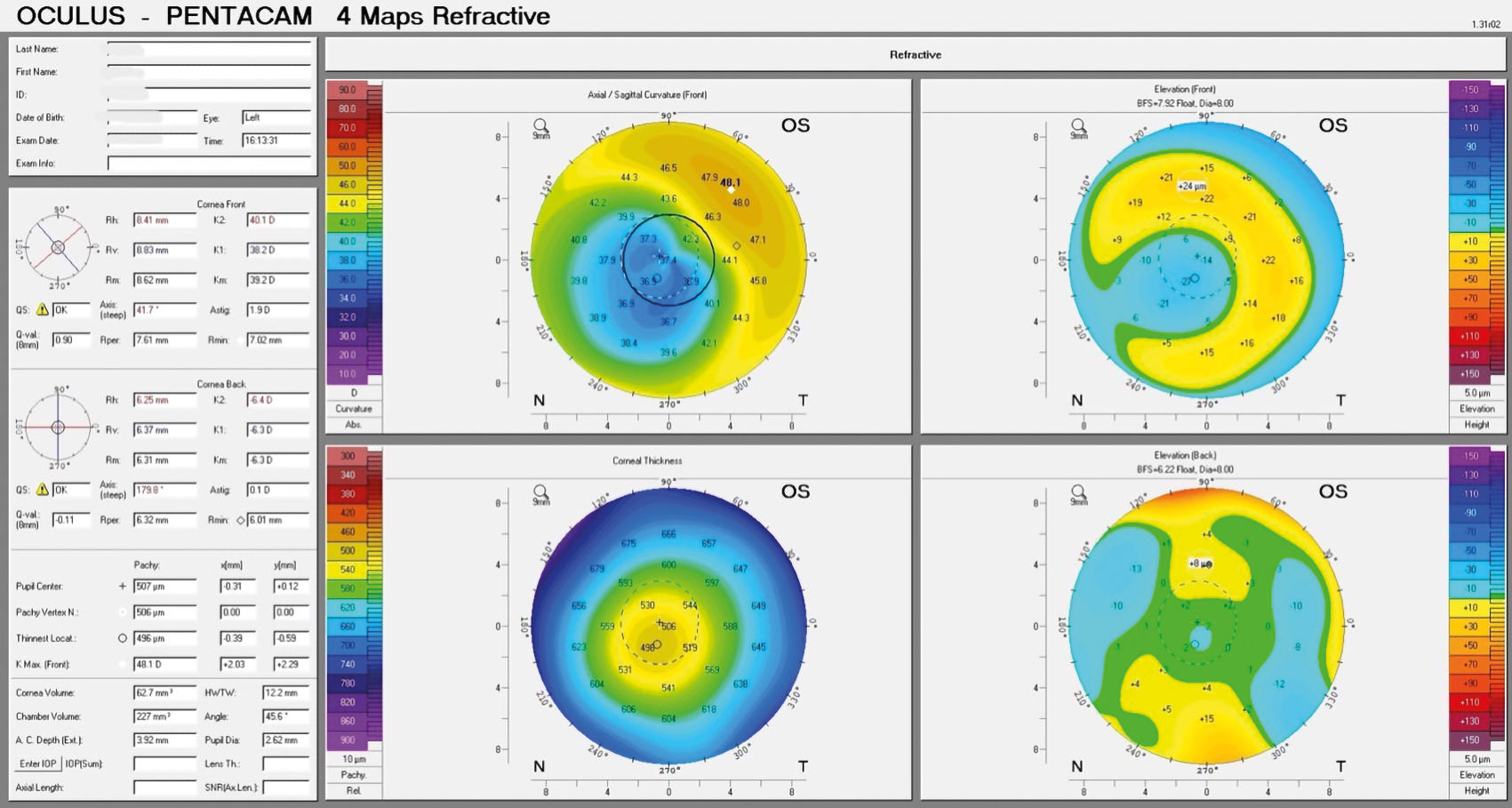
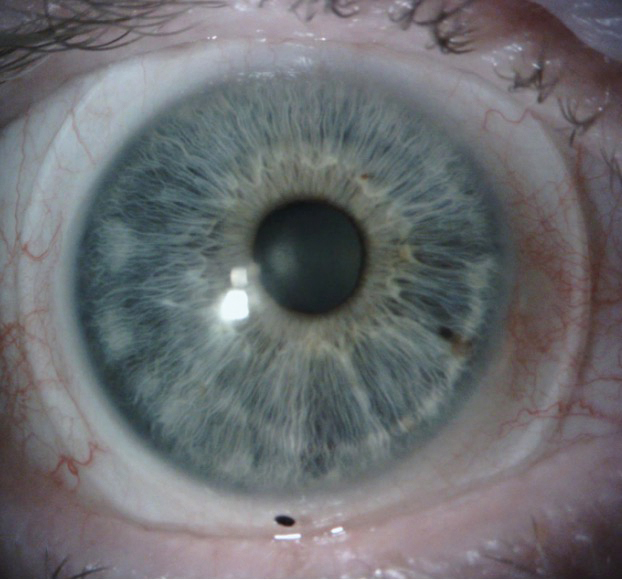
A 63-year-old Caucasian male presented with a chief complaint of blurry vision and “seeing 5 images” with and without spectacles for many years beginning after undergoing Lasik surgery OU that resulted in mild post-Lasik ectasia with OS more affected than OD (Figure 1). The patient’s history included no previous contact lens wear and two traumatic brain injuries due to two separate motor vehicle accidents, which occurred pre-LASIK surgery. Past magnetic resonance imaging (MRI) were reported to be normal. The patient had also been diagnosed with an epiretinal membrane OS result-ing in further mild distortions in vision OS.
The patient’s unaided acuities were 20/30-2 OD, 20/30-1 OS, and 20/30 OU with subjective complaints of shadowing and multiple images in each eye, with OS being more noticeable. The Pentacam corneal topography and pachymetry confirmed irregular astigmatism and showed corneal thickness to be 509 µm OD and 496 µm OS. The pres-ence of a binocular vertical imbalance was noted. Preliminary testing indicated otherwise normal ocular health. Anterior segment biomicroscopy reflected the surgical history with Lasik flaps OU but was otherwise unremarkable.
Treatment and Management
At the initial visit, a new scleral lens fit was started OU with 16.8 mm overall diameter Custom Stable (Valley Contax, Eugene, Oregon) lenses to vault the irregular cornea and limbus, correcting the patient’s irregular astigmatism. At the first lens dispense, vertical, binocular diplopia was reported with the scleral lenses that was not noticed before by the patient. Further binocular vision testing while wearing the scleral lenses was performed and showed a 3 prism diopter (pd) right hypertropia due to a longstanding fourth nerve (CN IV) palsy secondary to above mentioned trauma. The patient achieved single vision with 3 pd base down (BD) prism OD with trial frame over the lenses. According to the manufacturer of the lenses, the lathing of scleral lenses limits prismatic correction to 4 pd per lens in 1 direction, so a new scleral lens was ordered with the 3 pd BD prism incorporated OD.
At the first lens dispense and follow up, the patient’s diplopia was improved, but was still noticeable to the patient, so additional binocular vision testing was performed over the prism scleral lenses. Using a Modified Thorington test, a technique which measures phorias and tropias using a scale and a Maddox rod, the patient showed alignment with 1 pd of additional BD OD.
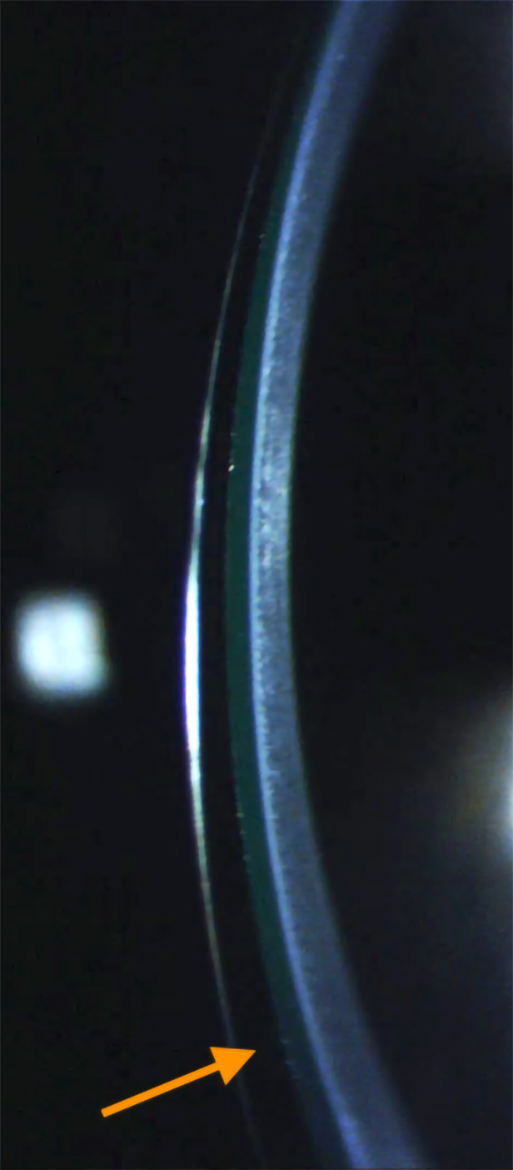
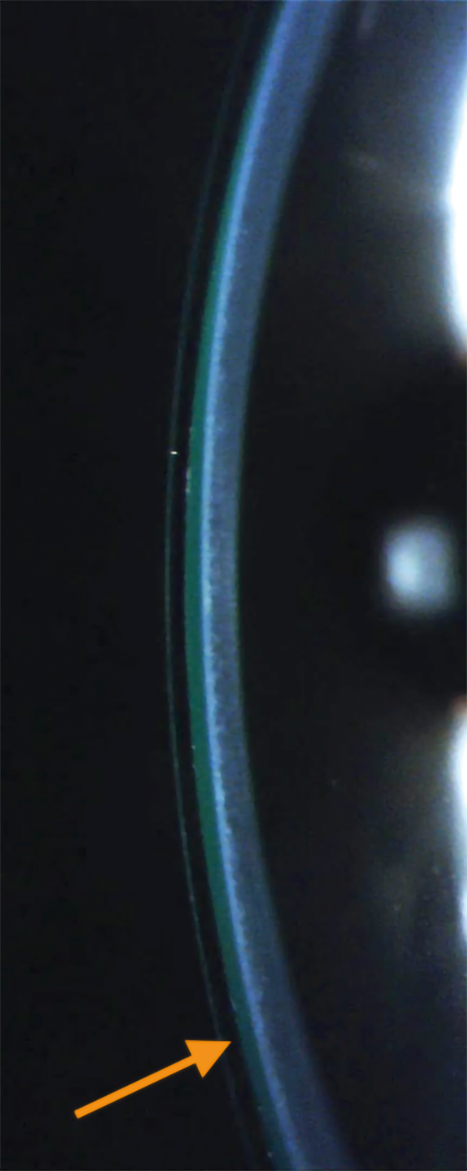
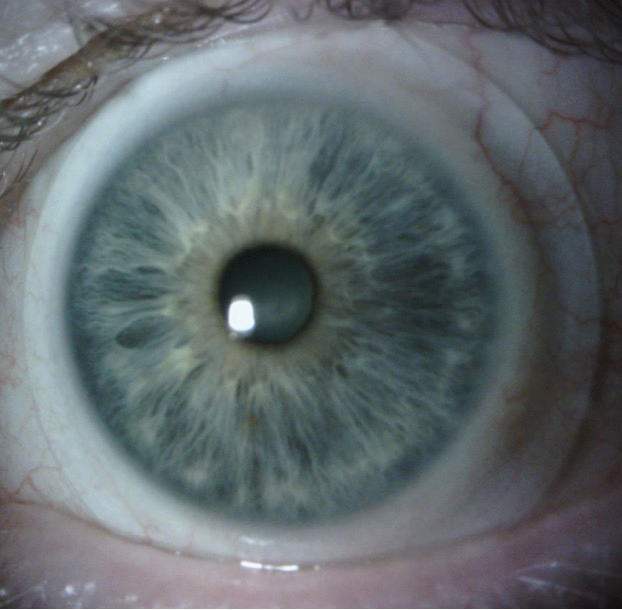
At the second lens dispense and follow up, the patient achieved clear and single vision with the 4 pd BD lens OD (Figure 2, Figure 3). The prism was then split into 2 pd base down OD and 2 base up OS to achieve a thinner lens thickness OD from 0.54 mm to 0.38 mm. The vertical landing zone was also steepened to assist in lens centration and rotational stability. The gas permeability of the lens was increased from 100 to 180 as well to compensate for the reduction in oxygen transmittance due to increased lens thickness from the incorporation of prism.
The patient achieved clear, single vision and a rotationally stable and acceptable fit with the final dispensed scleral lenses. The final lens parameters for the OD lens were a diameter of 16.8 mm, a base curve of 8.04 mm, a sag of 5.157 mm, with a power of -5.25 D. Center thickness was 0.38 mm, the flat scleral landing zone was 3.00, and the steep landing zone was -6.00 with 2 pd BD. For the left eye, the diameter meas-ured 16.8 mm, the base curve was 8.04 mm, with a sag of 5.158 mm, with a power of -5.50D, a center thickness of 0.37 mm, a flat scleral landing zone of 3.00, and a steep landing zone of -6.00, with 2 pd BU. The final lens material for both lenses was tisilfocon A OU. Final scleral lens acuities were 20/20 OD, OS, OU with single and binocular vision.
The ultrahigh Dk material allowed for all day wear of the contact lenses without end of the day hazy vision.
Discussion
Strabismus affects 2 % to 5 % of the general population.2 Patients within this population may also be affected by irregular astigmatism from conditions such as post-refractive ectasia, keratoconus, trauma, and corneal surgery. The incidence of post-Lasik ectasia is reported to be 90 per 100,000 eyes.3 In the present case, with concomitant ectasia and heterotropia, the patient was able to achieve relief from both irregular astigmatism and diplopia using scleral lenses with prescribed prism. Unlike other contact lens options, such as soft or gas permeable corneal lenses, scleral lenses have the unique ability to be rotationally stable even with prescribed prism in any direction using toric, quadrant specific, or impression and scan based “free-form” peripheral curves, with “free-form” being the most stable.1,4,5 Adequate centration of the scleral lens is also important in lenses with prism because decentration induces unintended prismatic effects.1
Higher Dk materials and a limited central fluid reservoir of no more than 200 microns should be considered in the use of scleral lenses with prescribed prism due to the increased central thickness of the lens.6,7 The ideal central lens thickness in a scleral lens should not exceed 250 microns.7 Factors that increase a scleral lens’ central thickness include: overall diameter, the refractive power of the lens, material, and prism.7 Prescribing prism in a scleral lens increases central lens thickness substantially. In this particular case, a 4 pd lens was 0.54 mm thick centrally while a 2 pd lens was 0.38 mm thick when a standard lens with a similar power to the present case without prism is typically around 0.2 - 0.25 mm. If this patient required hyperopic correction in the scleral lens, the central thickness would be even thicker. When prism was reduced from 4 pd to 2 pd, the lens thickness was reduced by nearly 50 %. Also, lens flexure from the higher Dk material in lenses with prism is less of a concern due to the increased thickness from the prism. Obtaining well aligned peripheral haptics, which is needed in a stable prism scleral lens, decreases scleral lens flexure as well.8
The multiple images experienced by the patient were not all due to heterotropia, but in part were caused by irregular astigmatism provoked by corneal ectasia which in this case was mild and caused modest irregular astigmatism. Despite Lasik surgery, the corneal thickness was within the range considered normal for both eyes / OU. In the present case the scleral lenses were effective in masking these ghost images reported by the patient. In cases where the scleral lens is not eliminating such diplopia, high order aberration correction should be considered.
Conclusion
In patients with irregular astigmatism and diplopia correctable with a low amount of prism, scleral lenses should be considered for their dual benefits over other lens types which require the use of spectacles over the contact lenses. The cosmetic advantage of contact lenses should not be underestimated and, therefore, patients with regular corneal astigmatism requiring low magnitudes of prism may indeed benefit from scleral lenses as an alternative to prism in spectacle lenses.
Conflict of Interests:
The authors declare that there is no conflict of interests re-garding the methods and devices mentioned in the article.