Visual Quality Indicators with Multifocal and Dual-Focus Soft Contact Lenses for Myopia Control
Purpose: The purpose of this study was to determine and compare visual quality indicators in eyes wearing multifocal center-distance, and dual-focus soft contact lenses that are specifically designed for the purpose of myopia progression management, as well as single-vision soft contact lenses.
Material and Methods: Visual quality indicators of eyes of 34 healthy, young myopic adults ages 20 to 35 were determined. Non-cycloplegic measurements were conducted without contact lenses (baseline) and while subjects wore soft multifocal center-distance soft contact lenses (ArtMost SoftOK SMR and SEED 1-day Pure UP Multistage daily disposable), dual-focus soft contact lenses (CooperVision MiSight 1 Day), and single-vision soft contact lenses (iLens Aqua Bi-weekly). In this study, the lenses were referred to as SoftOK, Pure UP, MiSight, and iLens. The measured and analyzed visual quality indicators included high-contrast distance and near visual acuity, stereopsis, accommodative amplitude, accommodative response, spherical aberration, and horizontal coma.
Results: High-contrast distance and near visual acuities, accommodative responses, and stereopsis values achieved with the SoftOK, Pure UP, and MiSight contact lenses were comparable to those achieved with the iLens single-vision soft contact lenses and to baseline values. Accommodative amplitude was slightly reduced with the MiSight contact lens and spherical aberration was significantly higher with the SoftOK lens compared to the other lenses. Both findings had statistical significance (P = 0.047 and P < 0.001, respectively). Horizontal coma, most likely resulting from slight lens decentration, was higher and more variable with the SoftOK lens compared to the other lenses, although no statistical significance was determined.
Conclusion: Dual-focus and multifocal center-distance soft contact lenses allow for good visual quality, especially clear vision at distance and near. Small differences in accommodative amplitude and spherical aberration were found between lens designs, however the clinical impact requires further investigation.
Introduction
Myopia is a type of refractive error in which distant images are focused in front of the retina. It is also a common cause of vision loss.1 In 2016, Holden et al. predicted that by the year 2050 the prevalence of myopia increases to 49.8 % of the world’s population and that 9.8 % would be affected by high myopia, which poses a significant risk of developing eye diseases such as myopic maculopathy and retinal detachment.2 In order to prevent the risk of eye diseases caused by myopia, controlling its progression has become an important topic for eye care practitioners in the past years.3
According to animal experiments, a myopic peripheral defocus induced by wearing plus power lenses can reduce the elongation of axial length.4 Smith et al. found that the image quality at the peripheral retina has a larger impact on refractive development than the image quality at the central retina.5
A more negative refractive error, longer axial length, and a more hyperopic relative peripheral defocus may be used to predict the onset of myopia.6 Faria Ribeiro et al. concluded that relative peripheral hyperopia defocus can be used to predict the progression of myopia, however, not all authors agree with this conclusion.7,8 Kang et al. state that a degree of peripheral retinal myopic defocus may be required for effective myopia control that is greater than habitually experienced.9
Orthokeratology effectively reduces both the progression of a myopic refractive error as well as reduces axial elongation.10 This treatment modality involves the overnight use of rigid, gas-permeable contact lenses with reverse geometry designs. It is known to produce corneal shapes that correct the distance refractive error centrally and provide increasing positive power values that correspond to the location of the periphery of the optic zones of the orthokeratology lenses. These corneal shapes create relative peripheral myopic defocus values.11 A hallmark of orthokeratology is that the peripherally induced positive power dynamically changes with the amount of myopia, which means the higher the corrected myopia, the higher the induced positive power, or add power.12
The concept of peripherally increasing positive power, present during orthokeratology, has also been applied to the design of soft multifocal contact lenses. Multifocal center-distance contact lenses possess a central zone of distance power with a progressive increase in positive power toward the periphery of the optic zone where the required add power is established. In contrast, dual-focus lenses have a central distance zone, surrounded by multiple concentric alternating zones of add power and distance refractive power. Studies with children showed that wearing multifocal, center-distance contact lenses and dual-focus contact lenses can reduce myopia progression and delay axial elongation compared to wearing single-vision contact lenses.13,14 Based on findings of the BLINK study, Walline, et al. suggested that a higher add power may result in a better myopia control effect.15
Ocular wavefront aberrations are typically expressed as Zernike polynomials and are grouped into lower-order aberrations and higher-order aberrations. Higher-order aberrations typically reduce retinal image quality and may provide optical signals that contribute to the regulation and modulation of eye growth and refractive error development. The magnitude and type of higher-order aberrations vary with age, refractive error, and during near work and accommodation.16 Some studies show that myopic eyes show significantly higher levels of ocular higher-order aberrations than emmetropic eyes, but others have found no differences.17–19 Several studies reported a significant negative correlation between spherical aberration and axial elongation in school-age children.16 In this context, it has been suggested that the presence of wavefront aberrations in human eyes is linked to the development of the refractive status, however, the findings of different studies are inconclusive.16,20,21 Higher-order aberrations with analytical significance in eyes wearing contact lenses are spherical aberration and horizontal coma.22,23 A multifocal contact lens design that provides a progressive increase in positive power across the wearer‘s entrance pupil will result in an increased amount of positive spherical aberration. Therefore, this design provides an extended depth of focus.24 This feature might be beneficial for controlling myopia progression. Coma is often associated with a decentered contact lens fit, typically causes a reduction in visual quality, and can be limited by selecting an appropriate contact lens design and adequate fitting parameters.25
With the continuous innovation of multifocal and bifocal contact lens designs, it was pointed out that poor visual quality is one of the possible reasons for myopia progression.26 Visual quality is generally influenced by visual acuity, contrast sensitivity, aberrations, stereopsis, glare, visual field, accommodative amplitude, and accommodative response.
As far as high-contrast visual acuity is concerned, Schulle et al. found no significant difference between single-vision spectacle lenses and Biofinity center-distance soft multifocal contact lenses with +2.50 D add power if the distance power of the multifocal contact lenses is increased by −0.50 D to −0.75 D.27 Gong, et al., however, indicated that besides better accommodative amplitude and accommodative facility, single-vision contact lenses provided improved visual acuity, contrast sensitivity, and phoria status compared to Biofinity center-distance multifocal contact lenses with +2.50 add power in high and low illuminance settings. In addition, wearing multifocal contact lenses resulted in reduced accommodative responses and increased exophoria when compared with single-vision contact lenses.28 In their study, Kang et al. found a reduction in the quality of vision with Proclear center-distance multifocal soft contact lenses with add powers of +1.50 and +3.00 D compared to that offered by single-vision soft contact lenses.29 This reduction was dependent on the add power in a way that higher add powers were associated with lower quality of vision. Kollbaum et al. compared visual acuities obtained with best spectacle distance correction, Proclear center-distance multifocal soft contact lenses with +2.00 add power, and MiSight dual-focus lenses. While both contact lens designs resulted in reduced visual acuity in low-illumination and low-contrast environments, the authors found no discernible differences between the two lens types.30 Ruiz-Pomeda et al. reported no change in accommodative function in children wearing the MiSight dual-focus contact lenses compared to single-vision spectacle lenses.31 Gifford et al. investigated accommodative responses in myopic adults when wearing Biofinity center-distance contact lenses, utilizing +1.50 D and +2.50 D add power values, NaturalVue aspheric center-distance multifocal soft contact lenses, and MiSight dual-focus contact lenses. They report that independent of the add power, accommodative responses were approximately 1.0 D lower across the stimulus range with the aspheric multifocal contact lenses.32
To assure patient satisfaction, compliance, and successful long-term use of multifocal or dual-focus contact lenses, good visual quality is important.
Based on the suggestions and variable findings of previous studies, the purpose of this study was to determine and compare visual quality indicators in eyes wearing multifocal center-distance, and dual-focus soft contact lenses that are specifically designed for the purpose of myopia progression management and single-vision soft contact lenses.
Methods
A single-blind, randomized prospective study was conducted to determine visual quality indicators in healthy, young myopic adults wearing two different types of multifocal, center-distance soft contact lenses, one dual-focus soft contact lens, and one single-vision contact lens. Since this study investigated visual function with and without contact lenses and not myopia progression, the outcomes can be extrapolated to children and adolescents. All measurements were conducted using best-corrected subjective refractions without contact lenses (referred to as baseline values) and with appropriately powered contact lenses based on the refractions vertex-corrected spherical equivalent powers. The visual quality indicators of interest were high-contrast distance and near visual acuities, accommodative amplitude, accommodative response, stereopsis, spherical aberration, and horizontal coma.
Research subjects
Healthy adults of ages 20 to 35, free of systemic or ocular disease, who were recruited from the Chung Shan Medical University, Taichung, Taiwan, participated in this study. The inclusion criteria were myopia ≥ −6.00 D, astigmatism ≥ −1.00 D, monocular and binocular high-contrast visual acuity ≤ 0.1 logMAR, and normal binocular visual function. The exclusion criteria were the current wearing of rigid contact lenses, eye surgery, eye-related diseases, and systemic diseases. A total of 34 subjects, 12 males and 22 females, were enrolled in the study. The average age of all subjects was 21.86 years (SD ± 2.14). The average spherical equivalent power values were −3.58 D (SD ± 1.68) for the right eyes and −3.45 D (SD ± 1.80) for the left eyes. All participants had previously used trial contact lenses. Habitual soft contact lens wearers ceased wear for at least 24 hours prior to the
measurements.
The study was conducted in accordance with the Declaration of Helsinki and informed consent was obtained from all subjects prior to their involvement in the study. Ethical approval was obtained from the Institutional Review Board of the Chung Shan Medical University Hospital, Taichung, Taiwan. (Approval number: CS2-20089).
Measurements of subjective refraction, accommodative amplitude, accommodative response, and stereopsis
A Topcon VT-10 phoropter (Topcon, Tokyo, Japan) and a View-M digital visual acuity chart (Quan Chin Industrial Co., Taiwan) were used to measure high-contrast visual acuity and distance subjective refraction. The subjective refraction procedure included hyperfocal refraction (maximum plus to maximum visual acuity, MPMVA), Jackson cross-cylinder, binocular balance, and duochrome test techniques. A TMV near point card (Brighten Optix Co., Taiwan) was used to measure high-contrast near visual acuity at 40 cm. The accommodative amplitude was measured using a binocular push-up test with an RAF ruler (Bernell Co., Mishawaka, IN). During this test, the subjects wore their subjective refractions in a trial frame. Each measurement was repeated three times and an average value was used. The accommodative response was measured with using a Topcon VT-10 Phoropter and a TMV Near Point Card at a distance of 40 cm, using the fused cross-cylinder method, whereby the near stimulus was a 0.1 logMAR letter size. The results were grouped into normal accommodation (+0.25 D to +0.75 D), accommodative lag (greater than +0.75 D), and accommodative lead (less than +0.25 D). Stereopsis was measured with a Titmus Stereo Test (Bernell Co., Mishawaka, IN). To assure consistency, all measurements were conducted with the same equipment by one examiner in the same examination room.
Measurements of objective refraction and ocular wavefront aberrations
A Shin-Nippon K5001 open-field autorefractor (Rexxam Co., Osaka, Japan) was used to determine an objective starting point for obtaining the subjective baseline refractions. The measurements were conducted without cycloplegia and to assure adequate pupil diameters, the room light was dimmed. All subjects were guided to fixate a luminous visual target whose size corresponded to a visual acuity of 0.3 logMAR. The fixation distance of the visual target was 7.5 meters.
A Nidek OPD Scan 3 wavefront aberrometer (Nidek Inc., Tokyo, Japan) was used to determine spherical aberration and horizontal coma without cycloplegia for a 5 mm pupil diameter.
Contact lenses, measurements over contact lenses, and wearing sequence
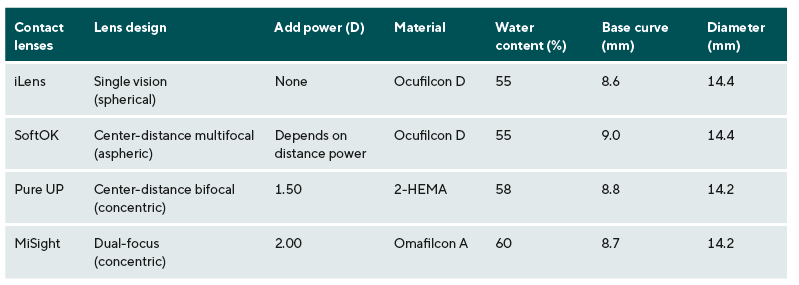
Four types of soft contact lenses were used in this study. The center-distance multifocal contact lenses were the ArtMost SoftOK SMR soft contact lens (Seinoh Optical Co., Taipei, Taiwan) and the SEED 1-day Pure UP Multistage daily disposable soft contact lens (SEED Co., Tokyo, Japan) with an add power of +1.50 D. The dual-focus contact lens was the MiSight 1 Day contact lens (Coopervision, San Ramon, CA). The iLens Aqua Bi-weekly soft contact lens (Seinoh Optical Co., Taipei, Taiwan) was the single-vision lens. Throughout this article, the different lenses will be referred to as follows: SoftOK (ArtMost SoftOK SMR soft contact lens), Pure UP (SEED 1-day Pure UP Multistage daily disposable soft contact lens), MiSight (MiSight 1 Day soft contact lens), and iLens (iLens Aqua Bi-weekly soft contact lens).
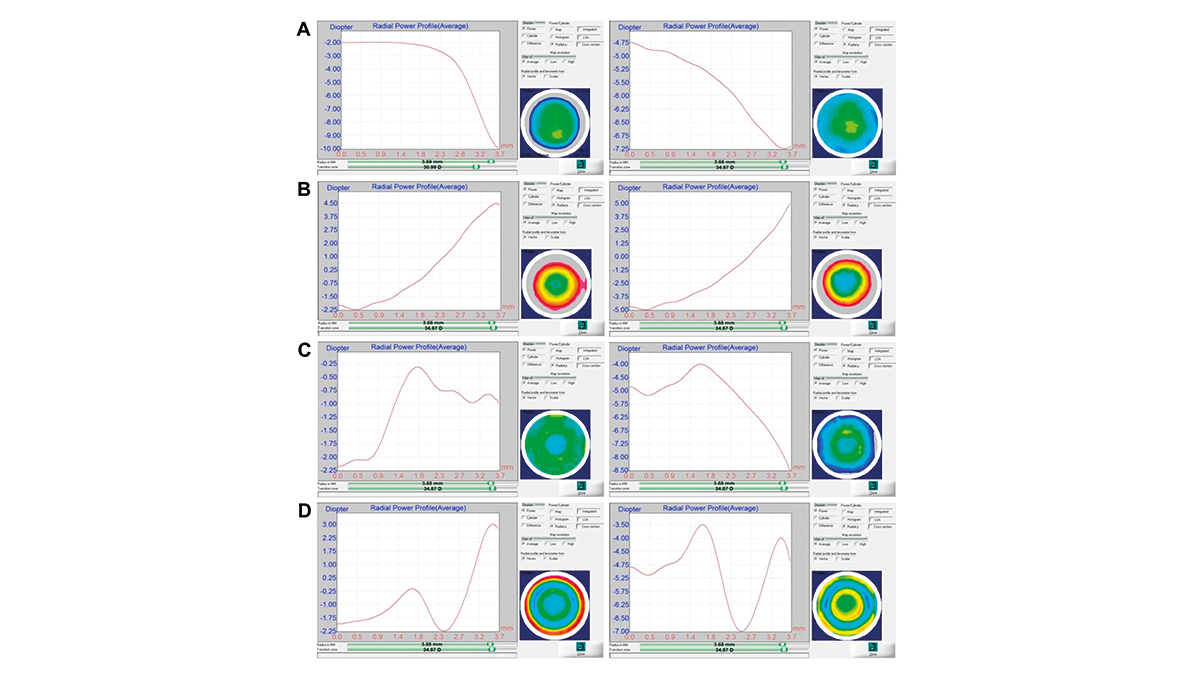
While the Pure UP contact lens and the MiSight contact lens had fixed additional power values of +1.50 D and +2.00 D respectively, the peripheral power of the SoftOK lens changed depending on its distance power. With an increase in the negative distance power of this lens, the peripheral power dynamically increased in a positive direction. Utilizing this design, the SoftOK lens aims to mimic the optical characteristics of a cornea during the process of orthokeratology. The MiSight contact lens contains a central correction zone surrounded by a series of treatment and correction concentric zones of alternating distant and near powers. Specifications of the contact lenses used in this study are listed in Table 1 and radial power value distributions of contact lenses with distance powers of −2.00 D and −5.00 D are displayed in Figure 1. These radial power profiles were measured with using a Contest Plus lens analyzer (Rotlex, Omer, Israel).
Each participant received a comprehensive eye examination. The distance power for each contact lens was determined based on the spherical equivalent power of the corresponding refractive error. The trial lenses were fitted and allowed to settle for 20 minutes. After the correct fit and adequate centration of each lens were confirmed, an over-refraction was conducted to determine the final lens power. A maximum decentration of 0.5 mm was accepted. The corresponding contact lenses were then selected for each participant.
Each type of contact lens was worn for a period of 4 days for a minimum of 6 hours and a maximum of 15 hours per day. The wearing sequence for the different contact lenses was assigned using permuted block randomization. The examiner prepared each set of contact lenses and handed them to the subjects in neutral containers to preserve the single-blind design of the study. At the end of each wearing period, visual quality indicators were measured, and a new lens pair was handed out.
Data analysis
Repeated-measure one-way ANOVA with Bonferroni post-hoc comparison was used to analyze continuous variables (distance and near visual, accommodative amplitude, spherical aberration, and horizontal coma) and chi-square analysis was used to analyze categorical data (accommodative response and stereopsis). Both analyses were performed using SPSS 26.0 statistical software (IBM Corp., Armonk, NY). A value of P < 0.05 was considered statistically significant.
Results
High-contrast distance and near visual acuities
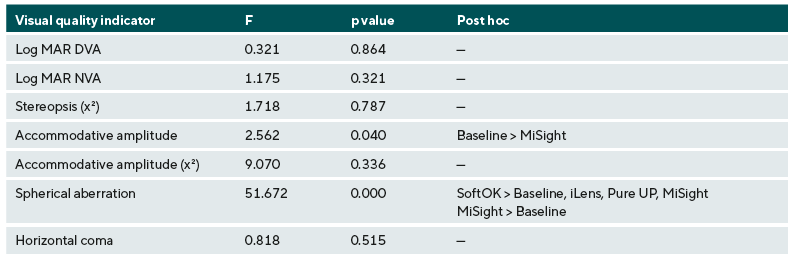
For the distance visual acuity, the average baseline value was −0.04 logMAR ± 0.05. When wearing the study lenses, the average values were −0.05 logMAR ± 0.05 for the iLens, −0.04 logMAR ± 0.05 for the SoftOK lens, −0.04 logMAR ± 0.04 for the Pure UP lens, and −0.04 logMAR ± 0.04 for the MiSight lens. One-way ANOVA analysis showed no statistically significant difference in distance visual acuity between baseline and the four contact lenses (F = 0.321, P = 0.864). For the near visual acuity, the average baseline value was 0.00 logMAR ± 0.06, 0.01 logMAR ± 0.04 for the iLens, 0.02 logMAR ± 0.05 for the SoftOK lens, −0.03 logMAR ± 0.05 for the Pure UP lens, and 0.01 logMAR ± 0.03 for the MiSight lens. One-way ANOVA analysis showed no statistically significant difference in near visual acuity between baseline and the four contact lenses (F = 1.175, P = 0.321).
Stereopsis
The average value of baseline stereopsis was 43.7 arcsec ± 6.6. When wearing the study lenses, the average stereopsis values were 41.6 arcsec ± 2.7 for the iLens, 40.5 arcsec ± 1.0 for the SoftOK lens, 41.6 arcsec ± 2.8 for the Pure UP lens, and 40.5 arcsec ± 1.0 for the MiSight lens. This indicates that all average values were clustered close to approximately 40 arcsec, which is considered a clinically normal value. For analysis, the data were grouped into 40 arcsec and less as well as greater than 40 arcsec. According to Chi-square analysis (χ2 = 1.718, P = 0.787), stereopsis was not significantly affected by the different lenses.
Accommodative amplitude
The average value of the baseline accommodative amplitude was 10.67 D ± 1.53. When wearing the study lenses, the average accommodative amplitude values were 9.38 D ± 1.21 for the iLens, 9.14 D ± 2.48 for the SoftOK lens, 9.89 D ± 2.97 for the Pure UP lens, and 8.88 D ± 2.34 for the MiSight lens. The data are visualized in Figure 2A. One-way ANOVA analysis showed a statistically significant difference between baseline measurements and measurements with the four lenses (F = 2.562, P = 0.040). Using Bonferroni’s post-hoc comparison, the MiSight lens showed a statistically significant change in accommodative amplitude compared to the baseline value (P = 0.047).
Accommodative response
The average value of the baseline accommodative response was 0.53 D ± 0.48. When wearing the study lenses, the average accommodative response values were 0.64 D ± 0.43 for the iLens, 0.49 D ± 0.28 for the SoftOK lens, 0.34 D ± 0.32 for the Pure UP lens, and 0.68 D ± 0.41 for the MiSight lens. As shown in Figure 2B, SoftOK, Pure UP, and MiSight lenses showed less variation. According to Chi-square analysis (χ2 = 1.718, P = 0.787), there was no statistically significant difference between the baseline values and the values measured with the four lenses.
Spherical aberration
The average value of the baseline spherical aberration was +0.0404 µm ± 0.0551. When wearing the study lenses, the average spherical aberration values were −0.0037 µm ± 0.0824 for the iLens, +0.2497 µm ± 0.0775 for the SoftOK lens, +0.0017 µm ± 0.0800 for the Pure UP lens, and −0.0469 µm ± 0.0910 for the MiSight lens. The data are visualized in Figure 2C. Since the baseline spherical aberration of the uncorrected eye will be changed after correction, only data obtained while wearing the four different contact lenses were analyzed. With this approach, one-way ANOVA showed a statistically significant difference between the four lenses (F = 51.672, P < 0.001). The high positive spherical aberration of the SoftOK lens was statistically significantly different from the spherical aberration values of the iLens (P < 0.001), the Pure Up lens (P < 0.001), and the MiSight lens (P < 0.001).
Horizontal coma
The average value of baseline horizontal coma was −0.0158 µm ± 0.0434. When wearing the study lenses, the average horizontal coma values were +0.0084 µm ± 0.0794 for the iLens, +0.0478 µm ± 0.2779 for the SoftOK lens,−0.0019 µm ± 0.0837 for the Pure UP lens, and +0.0003 µm ± 0.0877 for the MiSight lens. The data are visualized in Figure 2D. Since the baseline horizontal coma of the uncorrected eye will be changed after correction, only data obtained while wearing the four different contact lenses were analyzed. The average value for horizontal coma was substantially higher with the SoftOK lens and the standard deviation was wider than for any of the other lenses. One-way ANOVA, however, indicated that there was no statistically significant difference between the four lenses (F = 0.818, P = 0.515).

Discussion
Multifocal center-distance soft contact lenses have demonstrated their efficacy in decreasing the progression of a myopic refractive error as well as reducing axial elongation.13–15,33 While several studies described the optical characteristics of these contact lenses, especially the peripheral retinal defocus, few studies reported visual quality indicators associated with wearing these lenses. To analyze the latter was the purpose of this study. The measured visual quality indicators were high-contrast distance and near visual acuities, accommodative amplitude, accommodative response, spherical aberration, and horizontal coma.
In this study, no significant differences in high-contrast distance and near visual acuity were found between baseline measurements and when wearing the four study lenses. This is consistent with the research of Schulle, et al., Przekoracka, et al., and Ruiz-Pomeda et al. which suggested that center-distance multifocal contact lenses and MiSight dual-focus contact lenses should not cause significant changes in visual acuity or decline in vision.27,34,35
Stereopsis was also not affected by any of the contact lenses, which is consistent with the findings reported by Kang and Wildsoet for multifocal soft contact lenses and Ruiz-Pomeda et al. for the MiSight dual-focus contact lenses.31,36
In this study, an average reduction in accommodative amplitude by 1.79 D from baseline was found with the MiSight contact lens, which differs from the findings of Ruiz-Pomeda et al.31 In addition, the average accommodative response at baseline and with all study lenses were lower in the current study. A possible explanation for the different results is the difference in the ages of the subjects. While the average age in the current study was 21.86 years (SD = 2.14), the average age in the MiSight group in the Ruiz-Pomeda et al. study was 10.94 years (SD = 2.14). In addition, the methods used to measure accommodative responses differed in both studies. While the subjective fused cross-cylinder technique was utilized in this study, Ruiz-Pomenda et al. calculated the accommodative responses based on objective measurements obtained with a Grand Seiko WAM-5500 autorefractor.
A significant amount of positive spherical aberration was induced by the SoftOK lens. Cheng et al. suggested using soft contact lenses with positive spherical aberration to enhance the effectiveness of myopia control.37 This is based on the hypothesis that retinal hyperopic blur, caused by negative spherical aberration during accommodation, is a trigger for the progression of myopia. By design, a contact lens with positive spherical aberration can produce a shift of retinal hyperopic blur to the myopic direction while at the same time reducing relative peripheral hyperopia. Whether this translates into an enhanced myopia control effect of the SoftOK lens remains to be clinically verified.
The average value for horizontal coma was substantially higher for the SoftOK lens and the standard deviation was wider than for any of the other lenses, although there was no statistically significant difference between the four lenses. Coma-like aberrations typically result from lens decentration and have a detrimental effect on visual quality. Therefore, fitting strategies usually aim to reduce these aberrations. On the other hand, Hiraoka et al. analyzed ocular optical parameters in myopic children undergoing overnight orthokeratology and reported that the change in coma-like aberration was the most relevant variable to affect axial length. They concluded that asymmetric corneal shapes have a considerable effect on retardation of axial elongation and suggested that the inhibitory effect of orthokeratology on myopia progression is caused by mechanisms other than the reduction in peripheral hyperopic defocus.38 Since the SoftOK contact lens mimics the optical characteristics of a cornea during orthokeratology, the increased horizontal coma could be an associated finding. Whether this is somehow beneficial in controlling myopia progression remains to be investigated in future studies.
When performing aberration measurements, pupil size, environment setting, and equipment accuracy have a considerable impact on the collected data. While calibrated equipment was used for this study and standard measurement procedures were followed, there are several limitations to this study:
(1) Time constraints limited the measurements of visual quality indicators to periods of 4 days per lens type instead of repeated assessments over one or two years as reported in most myopia control studies.
(2) Due to the non-cycloplegic measurements, higher-order aberrations were recorded at pupil diameters of 5 mm, while other studies used 6 mm pupil sizes to evaluate ocular aberrations.
(3) Subjective visual quality indicators such as contrast sensitivity and the perception of halos and glare may be different when wearing multifocal contact lenses with different optical designs. These indicators were not assessed in this study.
(4) Stereopsis was measured with a traditional stereoscopic vision test that was limited to a minimum angle of 40 seconds of arc. Its accuracy might not be enough to produce true analytical differences.
While most visual quality indicators were not statistically significantly different for the various contact lenses investigated in this study, statistically significant differences were found for spherical aberration and amplitude of accommodation. Whether these differences may influence the efficacy of these contact lenses for controlling myopia progression, remains to be investigated in future studies along with the assessment of low-contrast visual acuity and visual function in dim illumination.
Conclusion
In this study, high-contrast distance and near visual acuities, accommodative responses, and stereopsis values achieved with the SoftOK, Pure UP, and MiSight contact lenses were comparable to those achieved with the iLens single-vision soft contact lenses and to baseline values. Accommodative amplitude was slightly reduced with the MiSight contact lens and spherical aberration was significantly higher with the SoftOK lens compared to the other lenses. Both of these findings had statistical significance.
In summary, dual-focus and multifocal center-distance soft contact lenses provide myopia progression control options while at the same time allowing for good visual quality, especially clear vision at distance and near. Differences in accommodative amplitude, spherical aberration, and horizontal coma may influence the myopia progression control with these lenses but requires further investigation.
Acknowledgments
This research was funded by Chung Shan Medical University (FCU/CSMU 109-003) in Taiwan.
COE Multiple Choice Questionnaire
The publication "Visual Quality Indicators with Multifocal and Dual-Focus Soft Contact Lenses for Myopia Control" has been approved as a COE continuing education article by the German Quality Association for Optometric Services (GOL). The deadline to answer the questions is 1st April 2024. Only one answer per question is correct. Successful completion requires answering four of the six questions.
You can take the continuing education exam while logged in.
Users who are not yet logged in can register for ocl-online free of charge here.