An Unusual Case of Vertical Pseudostrabismus
Purpose: This case report describes a rare case of vertical pseudostrabismus.
Material and Methods: A case of a four-year-old female patient is presented to evaluate the necessity of occlusion therapy. The treatment options are based on orthoptic and ophthalmological examination, as well as a review of the literature.
Results: The fully corrected visual acuity was 20/80 (logMAR 0.6) in the right eye and 20/200 (logMAR 1.0) in the left eye. Corneal reflex examination revealed a slight esotropia and a pronounced vertical deviation of the right eye (right over left). However, the cover test did not detect a misalignment. Fundus examination revealed retinopathy of prematurity with macular ectopia.
Conclusion: Vertical eccentric fixation is a rare condition. Therefore, treatment should be tailored to the patients’ needs.
Introduction
Pseudostrabismus refers to the apparent misalignment of the eyes without actual strabismus. This impression often arises in young children due to specific facial or ocular features, typically a broad nasal bridge. Strabismus is defined as a persistent deviation of the affected eye from the ortho position that cannot be corrected by a fusion stimulus. In contrast pseudostrabismus presents as an optical appearence of misalignment where both eyes remain parallel.
The exact incidence of pseudostrabismus is difficult to determine. Xu et al.1 reported a prevalence of approximately 4.2 % in the first year of life in Minnesota, whereas Ryu and Lambert 2 reported a prevalence of less than 1 % based on analyses of the Clinformatics Database (2003 – 2016). In over 96 % of cases, pseudostrabismus appeared as esotropia.1,2,3
In preterm infants with retinopathy of prematurity (ROP) and in inflammatory retinal diseases such as chorioretinitis, pseudostrabismus due to macular ectopia (where the central retina is displaced, altering the distance of the macula from the optic disc)4 has been described. The risk of strabismus and macular ectopia increases with the severity of ROP and the consequential interventions.5
Material and Methods
A four-year-old female patient, a former preterm infant born at 28 weeks of gestation, was referred for evaluation of occlusion therapy. Since birth, a vertical deviation of the right eye had been described. Previous occlusion therapy was alternated between the left and right eye due to inconsistent findings regarding ocular alignment and visual acuity. The patient had worn glasses since the first year of life to correct hyperopia and astigmatism, which she tolerated well.
Results
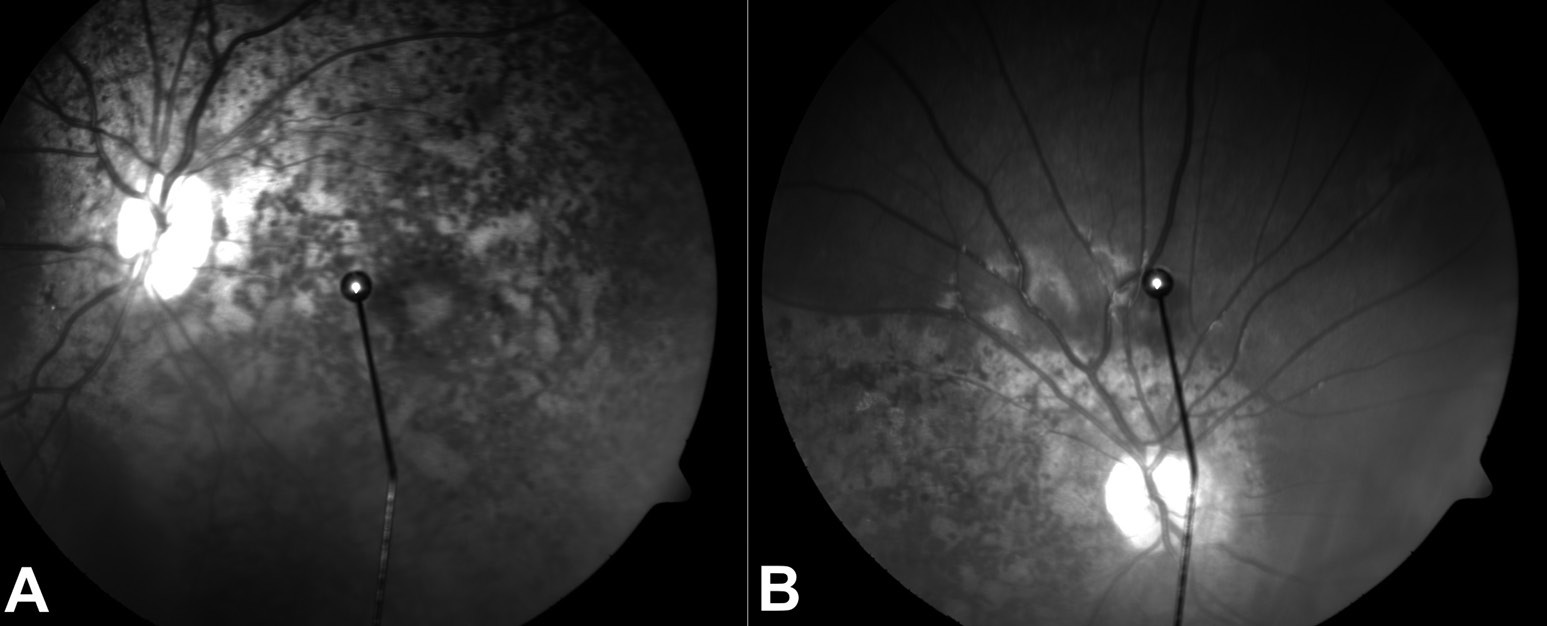
Visual acuity testing with Landolt rings 17.2´ showed 20/80 (logMAR 0.6) in the right eye and 20/20 (logMAR 1.0) in the left eye. The Hirschberg test revealed an upward and inward displacement of the corneal light reflex on the right side, while the left eye showed a small negative Kappa angle [nasal displacement of the reflex, (Figure 1)]. However, the cover-uncover test did not detect a misalignment. The translucent occluder test supported the suspicion of bilateral eccentric fixation. Visuoscopy confirmed bilateral eccentric fixation (Figure 2). Fundoscopic examination revealed ROP with absent macular structures of the right eye. In contrast, the left fundus exhibited macular structures. Optical coherence tomography (OCT) imaging of the macular structures at the fixation site was inconclusive in both eyes.
After consulting with the parents, we decided to continue occlusion of the right eye. This decision was based on the proximity of the eccentric fixation site and the presence of macular structures in the left eye. The aim of continuous occlusion was to weaken fixation in the left eye and to promote a more functionally retinal location as the new location of fixation. This strategy aimed to improve visual acuity of the left eye and encourage fixation switching to achieve a more normal ocular alignment.

Occlusion therapy was performed for 24 hours per day over the course of six weeks, with frequent follow-ups to prevent complications such as diplopia. Despite correct adherence to therapy, no changes of fixation or improvement of visual acuity were observed. This led to discontinuation of occlusion therapy after six weeks.
Discussion
Vertical eccentric fixations in childhood are extremely rare. Most documented cases in the literature date back to before 1960. In a review by Rados and Scholz,6 seven cases of vertical macular ectopia (displacement of macular structures upwards) were described, often due to chorioretinitis. Scheiman et al.7 reported 40 cases of macular ectopia, with 90 % involving temporal displacement. Similarly, Sahin Karamert et al.5 reported primarily temporal macular shifts in their patient population, mostly unilateral. Sahin Karamert et al. measured an average macular displacement of 6.22 mm (normal 4.7 mm)8, with individual cases ranging from 3 mm to a maximum of 13 mm. Visual acuity ranged from logMAR 0.5 to 0.6 [20/60 to 20/80 Snellen (ft)], although correlation between visual acuity and macular displacement was not specified.
The nasal macular displacement in our patient’s left eye, though rarer than temporal displacement in ROP, remains a recognized phenomenon. However, the location of fixation of the right eye and the corresponding visual acuity findings are noteworthy. In eccentric fixation, retinal structures remain intact, suggesting a maximum expected visual acuity of 20/200 – 20/125 (logMAR 1.0 – 0.8).9 Given that our patient’s right eye achieved a visual acuity of 20/80, macular ectopia in the right eye is likely. Detailed OCT imaging of the retinal structures would have been desirable.
The literature describes variable visual outcomes in cases of macular ectopia.5,6,10 Fabian et al.10 documented a case of vertical macular ectopia in the upper temporal artery region with full visual acuity.
Our therapeutic decision was based on the assumption that, in addition to visual impairment due to macular structural changes, amblyopia was also present. This condition, known as relative amblyopia, can only be confirmed retrospectively after occlusion therapy. Some authors report beneficial outcomes due to occlusion therapy despite severe organic changes and significantly reduced vision.11,12 Given the patient‘s age, prior occlusion treatments, and practical challenges in therapy implementation, continuous occlusion was chosen. This method remains controversial as prolonged disruption of binocularity might lead to strabismus and diplopia.13,14
During therapy, neither fixation changes nor visual acuity improvements of the left eye were observed. No side effects were reported. A hypothesized relative amblyopia of the left eye was not confirmed. The non-response to therapy suggests a more severe retinal damage than initially assumed.
Conclusion
Vertical pseudostrabismus is rare and always associated with fundus abnormalities. Occlusion therapy should be considered even in cases of macular ectopia, though success rates vary in the literature.
Conflict of Interests
The author declares that there is no conflict of interests regarding the methods and devices mentioned in the article.
zur Erlangung der Doktorwürde der Friedrich-Alexander-Universität
Erlangen-Nürnberg (Germany), https://open.fau.de/server/api/core/
bitstreams/18425bfb-c61d-41e7-91c2-6a1d7682f428/content. Referencing: 09 January 2025.
