Comparison of Refraction Data and Visual Acuity With and Without Cyclopentolate in Children and Young Adults
Purpose. This investigation compared refraction and visual acuity obtained under cycloplegic and non-cycloplegic condition in a Caucasian population.
Material and Methods. One eye of 73 subjects, aged 6-29 years, was examined under cycloplegic (C) and non-cycloplegic (NC) condition using autorefraction (AR), subjective refraction (SR) and visual acuity testing. Subjects were subdivided into refractive groups (emmetropia: −0.5 D < SE < +1.00 D, myopia: SE ≤ −0.5 D, hyperopia: SE ≥ +1.00 D).
Results. When comparing AR C and SR NC, deviations in SE were largest in hyperopes (∆SE = 0.74 ± 0.57 D; 95% CI: 0.5 – 0.97 D) compared to emmetropes (∆SE = 0.37 ± 0.21 D; 95% CI: 0.24 – 0.45 D) and myopes (∆SE = 0.25 ± 0.32 D; 95% CI: 0.12 – 0.38 D). When comparing SR C and SR NC, deviations in SE were largest in hyperopes (∆SE = 0.54 ± 0.43 D; 95% CI: 0.36 – 0.71 D) compared to emmetropes (∆SE = 0.23 ± 0.26 D; 95% CI: 0.10 – 0.35 D) and myopes (∆SE = 0.12 ± 0.17 D; 95% CI: 0.04 – 0.18 D).
In emmetropes and myopes, C and NC refraction did not change visual acuity. For hyperopes, visual acuity reduced by 0.38 ± 0.18 logMAR and 0.22 ± 0.18 logMAR when comparing AR C prescription and SR C prescription to SR NC prescription, respectively.
Conclusion. In emmetropes and myopes, C is not indicated. In hyperopes, C prescription may reduce NC visual acuity. For maximum visual acuity, a combination of C and subjective NC refraction is recommended. C refraction must be performed if visual abnormalities are suspected.
Introduction
Refraction represents an essential part of the eye examination. It is beneficial for the detection of refractive errors that, uncorrected or inappropriately corrected, lead to poor visual outcomes. It is well known that unrecognized, uncorrected strabismus and anisometropia are the most common causes of amblyopia in children worldwide.1,2 Furthermore, besides cataract and age-related macular degeneration, uncorrected refractive error is one of the most common causes of blindness and vision impairment in adults.3 Accordingly, different techniques have been evolved to determine the proper refraction and correction for optimal vision. These include objective and subjective methods, such as autorefraction and subjective refraction, with or without the additional use of cycloplegics. Relevant scientific and practical findings on these different methods are known. In optometric practice, the gold standard for evaluating the refractive error and the associated correction is subjective refraction.4,5 If subjective refraction is performed without cycloplegia, it is well known that myopia can be overestimated, and hyperopia underestimated.6 The findings on non-cycloplegic autorefraction are identical.7–15 Results of studies on children and young adults aged 7 to 21 years show that the difference between non-cycloplegic and cycloplegic spherical equivalents is statistically significantly higher in hyperopes than in emmetropes and myopes.16,17 A commonly discussed reason is accommodation.18 Particularly in pediatric populations, the accommodative system is very robust.19 If accommodation is not adequately relaxed, measured values may fluctuate.20 This may lead to inaccurate refractive measurements.19 Different methods exist to ensure accommodation control. These include the fogging technique, which is realized by optical lenses or integrated in autorefractometers.21–23 Despite the discussion about non-invasive techniques for accommodation control, cycloplegic measurement is preferred.24,22 Despite all the techniques available, cycloplegic refraction has become the gold standard to assess refractive errors in uncooperative subjects, children and adults up to 50 years, as well as in epidemiological studies.25–27,14,22,17,28,11
Accommodation, especially in children with a large accommodation range, but also in young adults, can lead to a so-called myopic shift and therefore have an impact on refraction.17 Cyclopegics are also used for indications such as children with fluctuating accommodation, patients with suspected pseudomyopia and accommodation problems including spasms, as well as children and adolescents with asthenopia.19 The use of cycloplegics can circumvent those issues. Cycloplegics have the effect of inhibiting the active accommodation response and releasing any accommodation spasm, by acting on the ciliary body as well as blocking the receptor site of acetylcholine.19 Therefore, refraction using cycloplegics is a common practice.17 Achieving full cycloplegia is essential for accurate measurements. In young subjects with high pigmented iris the sequestration of cycloplegic agents by the iris pigment may cause difficulties.30,31 The choice of an appropriate regimen in terms of choice of cycloplegic type, concentration and number of drops is essential. Several guidelines exist, however, they are intended for use in children.32–34 In general, the recommended cycloplegic is Cyclopentolate 1% as it inhibits accommodation quickly and effectively and has a comparatively short duration of effect. Depending on the specific case, other cycloplegics, such as tropicamide or atropine, are used. In addition to the inhibition of accommodation, temporary but also serious side effects may occur, such as blurred vision, drowsiness, ataxia and visual hallucinations.35,36 From practical experience, it is know that examinations with cycloplegic eye drops can be an unpleasant experience for children.
Worldwide, responsibilities and authorizations of optometrists differ. Such differences include the administration of diagnostic medications, such as cycloplegics, used for examinations. Throughout Europe, not all optometrists are authorized to perform cycloplegia without ophthalmic supervision. The use of cycloplegics by optometrists is prohibited in Asia, except for Singapore. The question remains whether it is generally necessary to perform cycloplegic refraction on all children. For the practical application, this study was designed to evaluate commonly used refraction (and correction) strategies, such as autorefraction and subjective refraction, under cycloplegic and non-cycloplegic condition in a Caucasian population. Furthermore, when prescribing corrections, visual acuity is a crucial parameter. Therefore, the effect of objective and subjective refraction with and without cycloplegia on visual acuity was investigated.
Methods
Study Design and Participants
This prospective cross-sectional study included 73 subjects. The mean age was 18.5 ± 6.2 years (range 6-29 years). 35.6 % of the subjects were male.
Recruitment was done through patients of a German optometrist and students, as well as acquaintances of the Ernst Abbe University of Applied Sciences Jena, Germany. The goal of subject recruitment was to achieve an even distribution of ametropias throughout the sample. Thus, comparable numbers of emmetropes, myopes, and hyperopes were assigned to the age groups 5 - 9 years (n = 10), 10 - 14 years (n = 14), 15 - 19 years (n =15), 20 - 24 years (n = 20), and 25 - 29 years (n = 14). Subjects were subdivided into the refractive groups according to their objective cycloplegic spherical equivalent (SE). The cycloplegic agent Cyclopentolate 1% was chosen to achieve cycloplegia. It was applied according to the instructions of the pharmaceutical supplier. One drop of the cycloplegic agent was administered twice after an interval of 15 minutes. Measurements were performed after an additional 20 minutes. Initially, SE was calculated for three autorefraction measurements under cycloplegic condition. The mean value was calculated to allocate the subjects to the corresponding group. The allocation of subjects into one of the three groups was done as follows: emmetropia: −0.50 diopter (D) < SE < +1.00 D, myopia: SE ≤ −0.50 D, hyperopia: SE ≥ +1.00 D.
The investigation was conducted according to the International Conference on Harmonization E6 Good Clinical Practice (ICH-E6 GCP). In addition, the study adhered to the principles of the Declaration of Helsinki for research involving human subjects and was approved by the Ethics Committee of the Friedrich Schiller University Jena, Germany.
Study Visit Overview
The investigation was done at the Ernst Abbe University of Applied Sciences Jena, Germany and Optik Hessler, Erlenbach am Main, Germany.
This study consisted of two examination appointments, which were 7 - 14 days apart. The same measurement procedures were performed on both appointments. One eye of each subject, randomly selected, was examined.
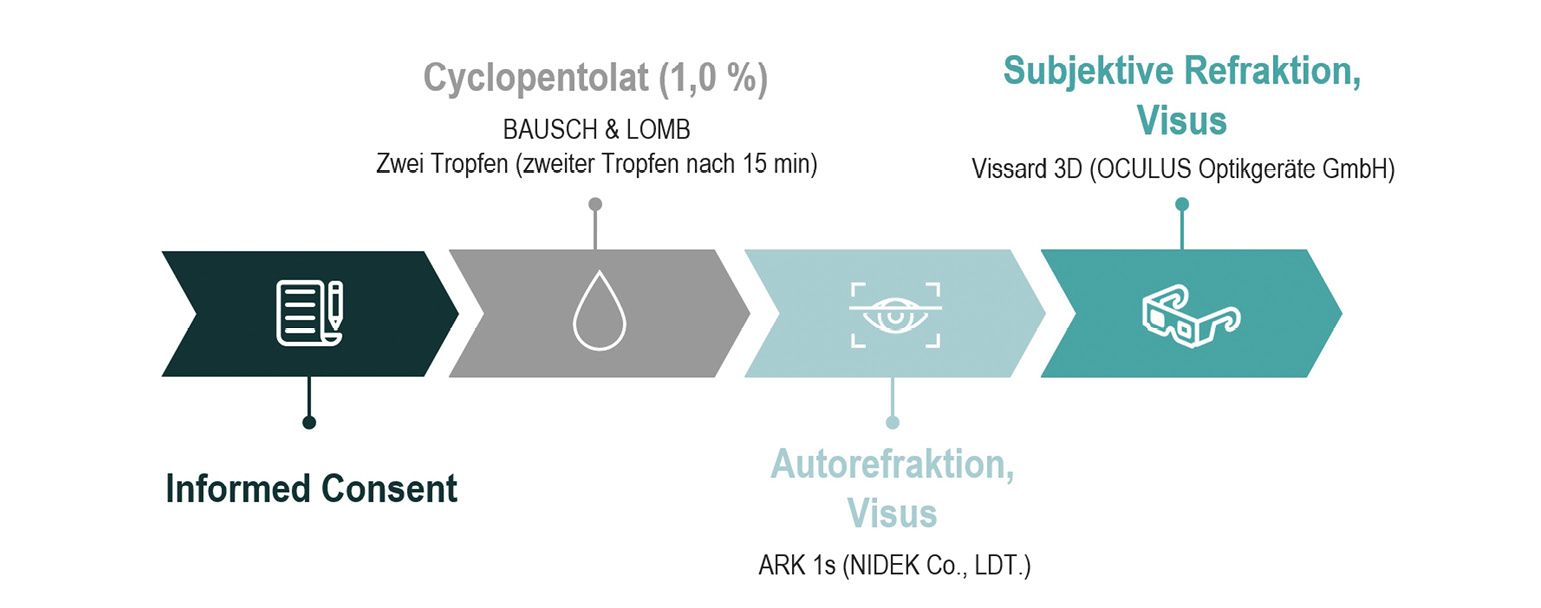
During the first appointment, subject information and consent were obtained, and inclusion and exclusion criteria, as shown in table 1, were evaluated. Subsequently, one drop of Cyclopentolate 1% was applied twice, 15 minutes apart. Measurements were recorded 20 minutes after the instillation of the last drop. As pigmentation of the iris was not an exclusion criterion, the investigator checked for sufficient pupil dilation prior to measurement to ensure that cycloplegia was achieved. Under cycloplegic (C) condition, autorefraction (AR) using ARK 1s (Nidek Co., Ldt.) as well as subjective refraction (SR) using Vissard 3D (Oculus Optikgeräte GmbH) and Universal Trial Frame UB 6 (Oculus Optikgeräte GmbH) was performed. Visual acuity was determined for both refraction results using the ETDRS chart. Figure 1 shows an overview of the first appointment.
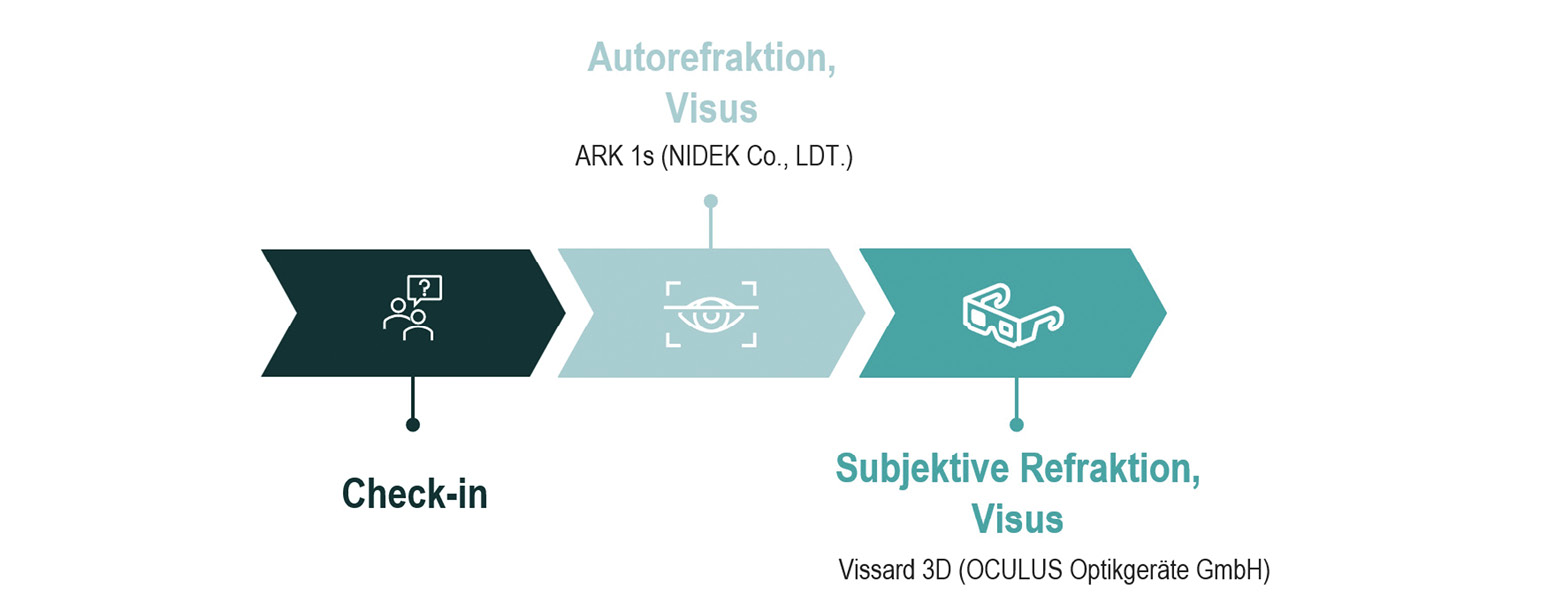
At the second appointment, AR and SR were performed under non-cycloplegic (NC) condition. Under NC condition, visual acuity was determined for refraction results previously obtained during AR C, SR C, AR NC and SR NC. As the measurement of visual acuity is performed without using cycloplegics to relax accommodation, a 5-minute period was permitted to adjust to C refraction. This period was chosen because there may be a tense accommodation, especially in hyperopic children, and a certain amount of time is needed to adjust to the prescription. Figure 2 shows an overview of the second appointment.
All objective measurements were performed three times. An average value was calculated.
High contrast monocular SR and logMAR distance visual acuity were measured at 6 m under photopic conditions. SR was determined with knowledge of AR and therefore as a refinement of AR. By default, a visual acuity level was considered successful as soon as 3 out of 5 optotypes were correctly identified. All measurements were done by one optometrist.
The primary outcome was SE in D.
The secondary outcome was visual acuity in logMAR.
To show the differences (∆) of SE determined under different conditions and using different measurement methods more clearly, the following determination was made:
(1) AR C and SR NC
(2) SR C and SR NC.
Statistical Analysis
To perform statistical analysis, SPSS Statistics 21.0 for Windows (IBM Corp., Armonk, NY, USA) was used.
Differences were calculated to show deviations in outcome measures obtained under cycloplegic and non-cycloplegic condition. Therefore, statistics included mean, standard deviation and 95 % confidence interval (CI). In addition, a boxplot diagram was used to present the differences of SE under different conditions in each refractive group. To determine the differences of SE in the refractive groups, ANOVA was performed. P-values less than 0.05 were considered statistically significant.
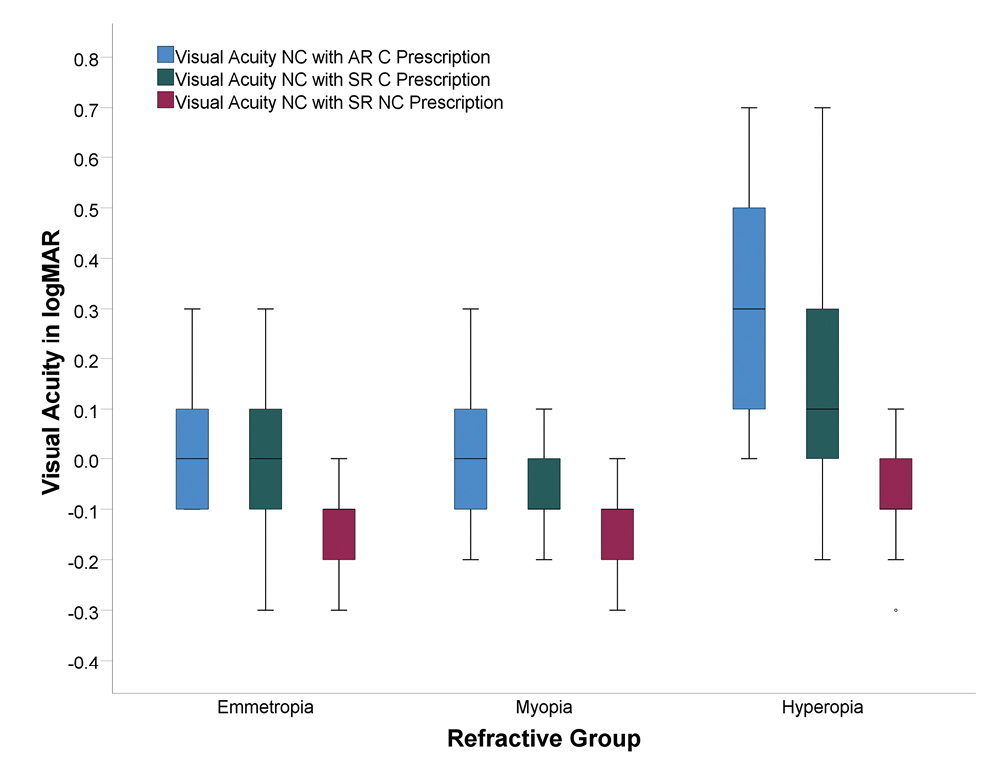
To present NC visual acuity achieved using different prescriptions in each refractive group, a boxplot was used. ANOVA was used to examine the correlation with age.
Intraclass correlation coefficient (ICC) and their 95% CI were used to evaluate reliability of objective measures under C and NC condition. Calculations were based on a mean-rating (k = 3), absolute agreement, two-way mixed-effects model. Values of less than 0.5, between 0.5 and 0.75, between 0.75 and 0.9 and greater than 0.9 indicate poor, moderate, good and excellent reliability, respectively.37
Results
Demographics
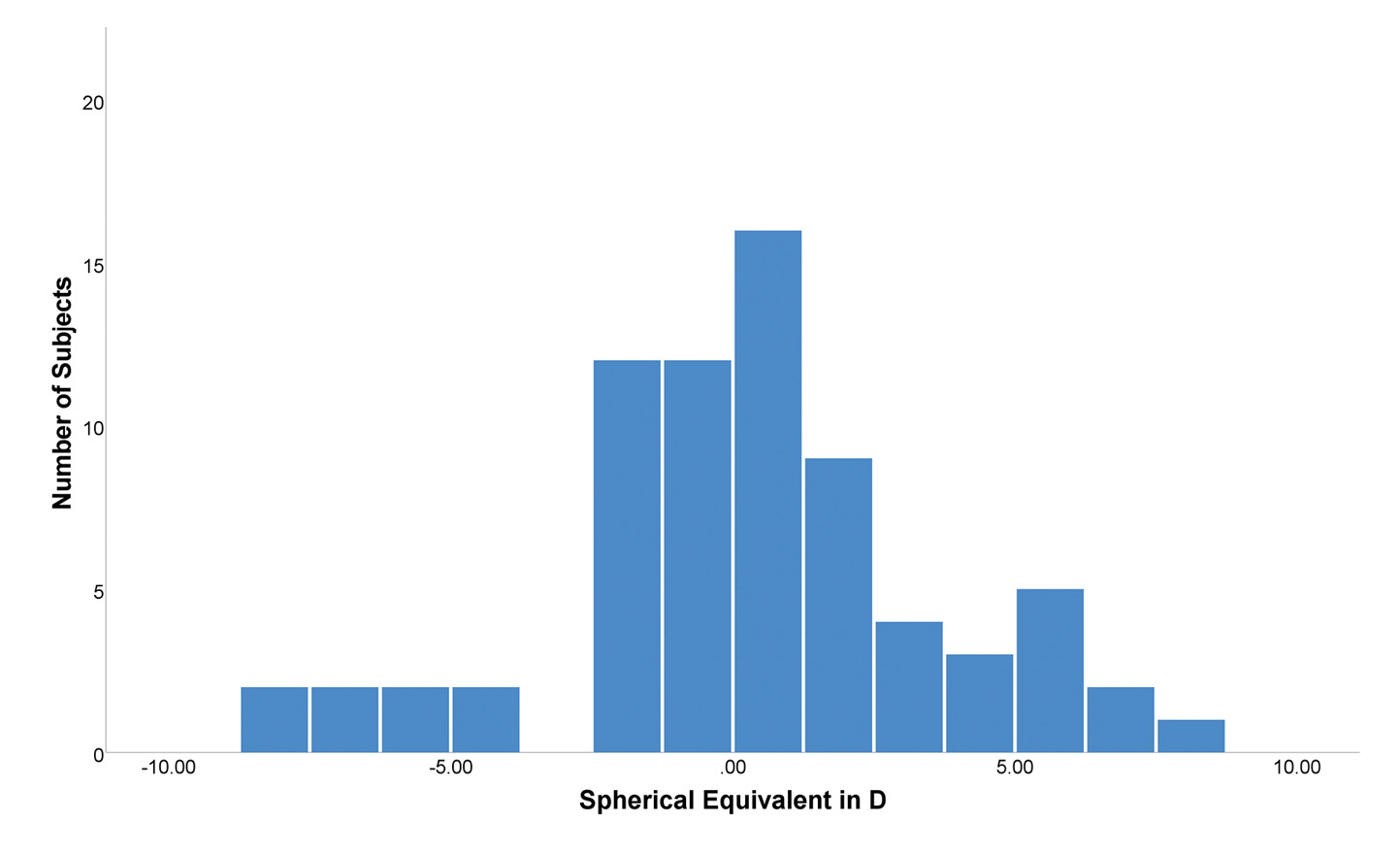
The sample had an objective cycloplegic SE of 0.27 ± 3.3 D, with −8.08 D being the minimum and 7.63 D being the
maximum.
Due to the specific recruitment, the representation of the three refractive groups was approximately equal with 30 %, 36 % and 34 % for emmetropia, myopia and hyperopia, respectively. The mean age was 19.4 ± 5.9 years for emmetropes, 18.4 ± 5.9 years for myopes and 17.8 ± 7.0 years for hyperopes. As the age distribution in each refractive group was similar, comparability of discrete results for the groups was given. The objective cycloplegic SE was 0.27 ± 0.45 D (range of 1.33 D), −3.02 ± 2.41 D (range of 7.42 D) and 3.55 ±1.99 D (range of 6.46 D) for the emmetropic, myopic and hyperopic group, respectively.
Spherical Equivalent
Regarding SE, reliability (ICC) for AR C and AR NC was 0.988 (95% CI: 0.982 – 0.992, P < 0.001) and 0.996 (95% CI: 0.995 – 0.998, P < 0.001), respectively. For both methods, ICC values greater than 0.9 indicated excellent reliability.
Figure 3 shows an overview of the deviations in SE determined under different conditions for each refractive group. More specifically, the hyperopic group showed the largest deviations in SE with (1) ∆SE = 0.74 ± 0.57 D, (2) ∆SE = 0.54 ± 0.43 D. The emmetropic and myopic group also showed deviations in SE with (1) ∆SE = 0.35 ± 0.23 D, (2) ∆SE = 0.23 ± 0.26 D, and (1) ∆SE = 0.25 ± 0.32 D, (2) ∆SE = 0.11 ± 0.17 D, respectively. The deviations in the emmetropic and myopic group were small compared to the hyperopic group. Table 2 shows the corresponding data, as well as the 95% CI.
When examining the differences in SE between the refractive groups, ANOVA showed a statistically significant difference between emmetropia and hyperopia, and between myopia and hyperopia with (1) P = 0.001, (2) P = 0.015, and (1) P = 0.002, (2) P < 0.001, respectively. There was no statistically significant difference between emmetropia and myopia with (1) P > 0.05 and (2) P > 0.05. Table 3 shows ANOVA results, including mean difference and 95% CI.
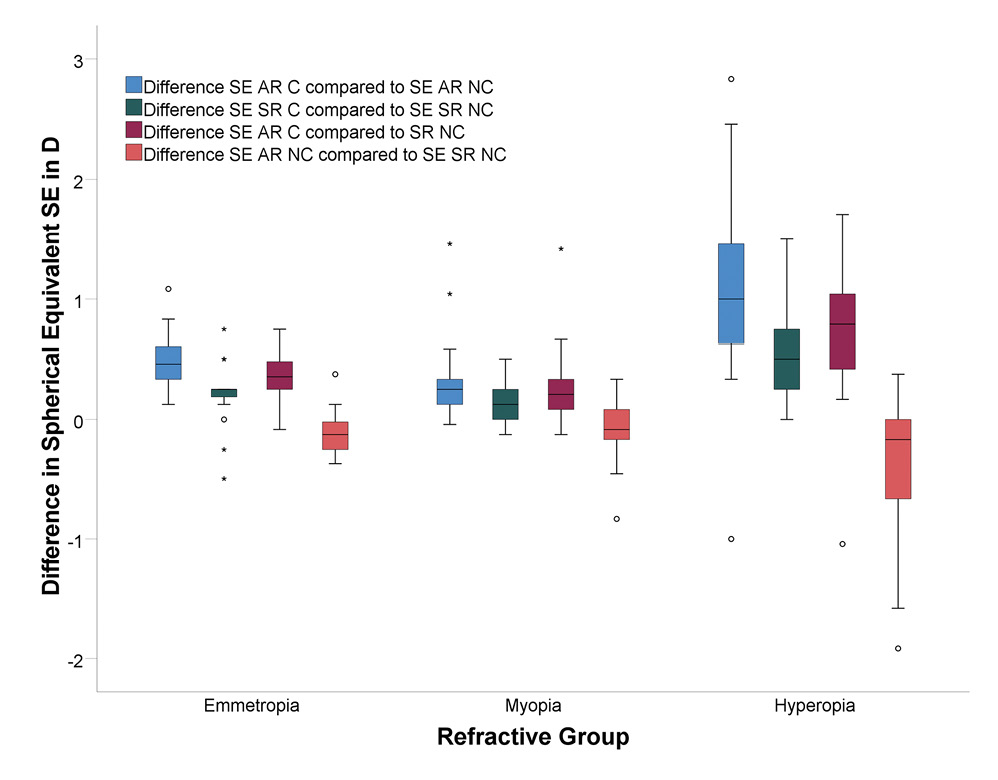
While looking through an optical instrument, inappropriate stimulation of accommodation may occur. Instrument myopia was calculated according to the equations of Salmon et al.38 Regarding SE, instrument myopia was negligibly low in emmetropes and myopes with 0.25 ± 0.19 D (95% CI: 0.16 – 0.34 D) and 0.21 ± 0.32 D (95% CI: 0.07 – 0.34 D), respectively. In myopes, higher values of instrument myopia were identified in only two subjects with 1.04 D and 1.21 D. Hyperopes showed higher values of instrument myopia with 0.57 ± 0.68 D (95% CI: 0.29 – 0.85 D) compared to emmetropes and myopes.
Visual Acuity
Figure 4 shows the outcome of visual acuity testing achieved under NC condition by each refractive group. Under NC condition, visual acuity was tested using each prescription (AR C, SR C, SR NC) determined during the examination appointments. In hyperopic subjects, using AR C prescription under NC condition, NC visual acuity decreased by 0.38 ± 0.18 logMAR compared to NC visual acuity achieved using SR NC prescription. Prescribing SR C values resulted in a decrease of 0.22 ± 0.18 logMAR in NC visual acuity. In emmetropes and myopes, regardless of the use of NC or C prescription, NC visual acuity did not change or changed only slightly compared to hyperopes. Table 4 shows the differences of NC visual acuity when using AR C prescription or SR C prescription compared to SR NC prescription.
Age
For each age group, table 2 shows data of the deviations in SE determined under different conditions for each refractive group.
Furthermore, ANOVA showed no correlation with age (P > 0.05). Accordingly, in each refractive group, no difference was found between young and older subjects in terms of NC visual acuity results.
Discussion
AR C and AR NC showed excellent reliability of SE measurements. Other studies on inter- and intraobserver agreement showed similar results.39–41 Furthermore, studies showed that AR NC provides comparable measurement results to SR NC.39,42,43 Accordingly, AR is a good estimate of SR. Nevertheless, if correction is prescribed, in addition to AR, SR should be performed.39,41
Similar to other studies, SE showed deviations when comparing C to NC values, with the largest deviations occurring in hyperopes.16,17 However, the results of this study showed that there was no critical deviation in refraction in emmetropes and myopes. When visual acuity was examined under NC condition using C and NC prescription, no significant difference was found in these two groups either. In hyperopes being under NC condition, visual acuity was reduced when using C prescription rather than NC prescription. The age of the subjects had no impact on the outcome.
The large deviations in SE, especially in hyperopes, have been proven to cause the decrease in visual acuity. In hyperopes, it can be assumed that (full) C refraction is not tolerated under NC condition due to poor visual acuity. This is expected to occur mostly in mild to moderate hyperopes.17 Due to the problem described, which is also confirmed by the results of this study, the prescription of full C refraction for hyperopes is not standard care. However, especially in Germany, there are no current standardized guidelines on a tolerable and appropriate modification of C refraction for hyperopes.
It is known to be biologically normal for the components of the visual system to change with age. Therefore, for the accommodative system, the same applies. After late childhood, the amplitude of accommodation decreases steadily.44 When comparing C and NC measurements, different amplitudes of accommodation could have an influence on the measurement result. Thus, it can be assumed that the differences of the measured values become smaller with increasing age (and associated decrease of accommodative ability). However, the results show no correlation with age.
In some cases, distinguishing between emmetropia and hyperopia can be challenging. To correctly identify the type of ametropia, a cycloplegic refraction is recommended. Thus, compensation by accommodation is eliminated. Hyperopia can be identified accurately. However, full C refraction may not be tolerated under NC condition. Also, estimating the extent of ametropia solely by distance visual acuity is error-prone, especially in hyperopes.45 Nevertheless, NC examination should be performed to find the best prescription for everyday life. To prescribe maximum plus values that achieve the best NC visual acuity, a combination of C and subjective NC examination is recommended.
According to the results of this study, relevant instrument myopia occurred exclusively in hyperopes. The cause may be the habitual tendency to overaccommodate, especially in young hyperopes.38 This is an additional reason why AR C in combination with SR NC is recommended to achieve the best correction for hyperopes.
In emmetropes and myopes, neither a difference in refraction nor in visual acuity was found under C and NC condition. Accordingly, to determine the prescription for the best visual acuity, standard refractions can be performed without cycloplegics in emmetropes and low to moderate myopes aged 6 – 29 years. Therefore, it is important to master accurate methods of refraction so that accommodation tonus/spasm does not affect the measurement.
In myopia management, prediction of myopia and initial diagnosis of myopia onset are important issues. In this regard, various ocular and nonocular predictive factors have been confirmed by studies. These include axial length, lens properties and corneal power, as well as parental history and activities outside of school.46–49 However, the most notable predictor is the refractive error.46,50 Children having a refractive error of +0.75 D or less at the age of 6 years are very likely to develop myopia.48 Therefore, the refractive error is determined under C condition.50 Results of this investigation showed no difference between C and NC refraction in emmetropes and myopes. Accordingly, consideration of NC refraction in myopia management seems possible. A combination of NC refraction and examination of other predictors is suggested.
C refraction must be performed if there are indications of visual abnormalities. These include accommodative esophoria, latent hyperopia, pseudomyopia, and amblyopia or their causative agents, strabismus and anisometropia. C examination provides reliable measurements that confirm or disconfirm the suspicion.51–55,33,34 C refraction may be considered prior to refractive surgery. Furthermore, examination under cycloplegia is useful if signs of asthenopia are present, especially in hyperopes.17
Existing studies show, that intraexaminer reliability is close to 80 percent agreement within ± 0.25 D for spherical equivalent.41 Nevertheless, one potential limitation to this study is the fact, that SR can be biased, eventhough the measurement is done by a trained optometrist, same as in this study. Also, SR was perfomed only once. This was due to time constraints. The results of repeated SR under different cycloplegic conditions could be investigated in a following study.
Individuals show different measurement results as soon as accommodation relaxes. Especially hyperopic children show significantly higher measurement results as soon as they adjust to new prescriptions. However, the time to release accommodation is different for each individual. There are no standard values. The relatively short time period used in this investigation may have caused bias. Accordingly, a longer period for the corresponding examination could lead to different results.
These statements are limited to a sample with an age range of 6 – 29 years. Investigation with the same research question on a sample with a wider age range of, e. g. 5 – 50 years, is recommended, since other studies show that differences were still found up to this age group.11
Due to the relatively small number of high myopic or high hyperopic subjects, as shown in figure 5, only limited conclusions on results of these subjects can be drawn. An investigation within the refractive groups remains of interest. Differences in high vs. low or mild myopia/hyperopia should be investigated. This requires a larger sample than the one presented.
Conclusion
The findings suggest that differences in SE are present when comparing C and NC condition. Hyperopes show the largest deviations in SE, which have an impact on visual acuity. Emmetropes and myopes show almost no differences in SE and visual acuity when C and NC condition are compared.
In conclusion for optometric practice, refraction under C condition is not indicated in emmetropes and myopes because there is no difference in refraction and visual acuity when comparing C and NC condition. In hyperopes, full C prescription may reduce NC visual acuity. If C refraction is performed, an additional subjective NC refraction is recommended.
Conflict of Interests
The authors declares that there is no conflict of interests regarding the methods and devices mentioned in the article.
Acknowledgement
Sincere gratitude to Andreas Glatz, M. D. for valuable contribution to the investigation.
144, 307–309.
Klaver, C. C. W., Logan, N. S., Naidoo, K., Resnikoff ,S., Sankaridurg, P., Smith, E. L. 3rd, Troilo, D., Wildsoet, C. F. (2019). IMI - Myopia Control Reports Overview and Introduction. Invest. Ophthalmol. Vis. Sci., 60, M1-M19.
