Short-term effect of Ortho-K on axial length and choroidal thickness
Purpose: To investigate the short-term effect of orthokeratology (ortho-k) on choroidal thickness (CHT), anterior chamber depth (ACD), central corneal thickness (CCT), and its relationship to the change in axial length (AL).
Material and Methods: Sixteen eyes of sixteen adult (age
25 - 54 years) ortho-k lens wearers discontinued treatment for one month. Measurements were taken before discontinuation, at the end of the break, and 2 - 4 weeks after resuming ortho-k lens wear. CHT was measured subfoveally and then nasally, as well as temporally of the fovea at 4 locations. Measurements were taken between 2 and 6 pm.
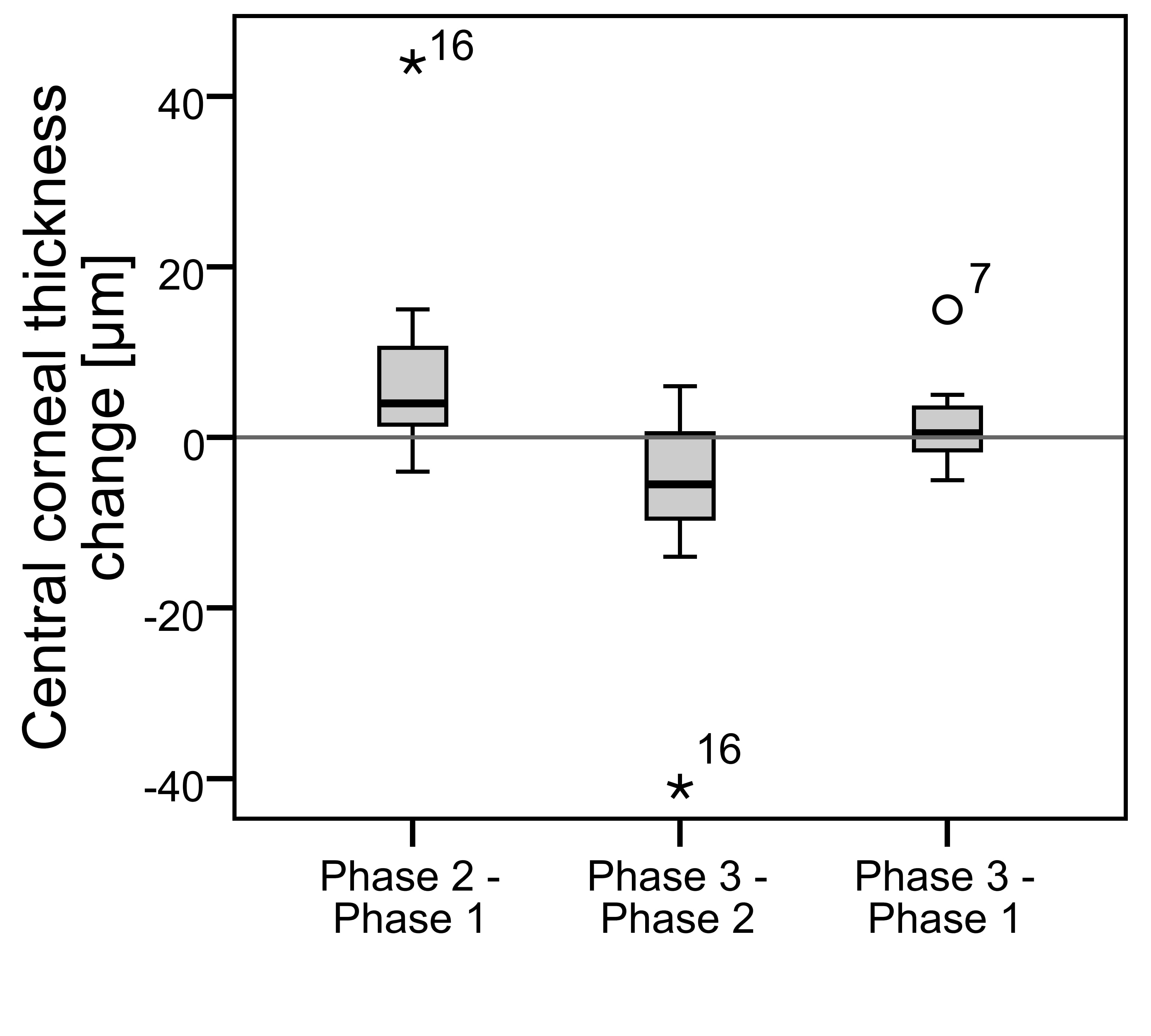
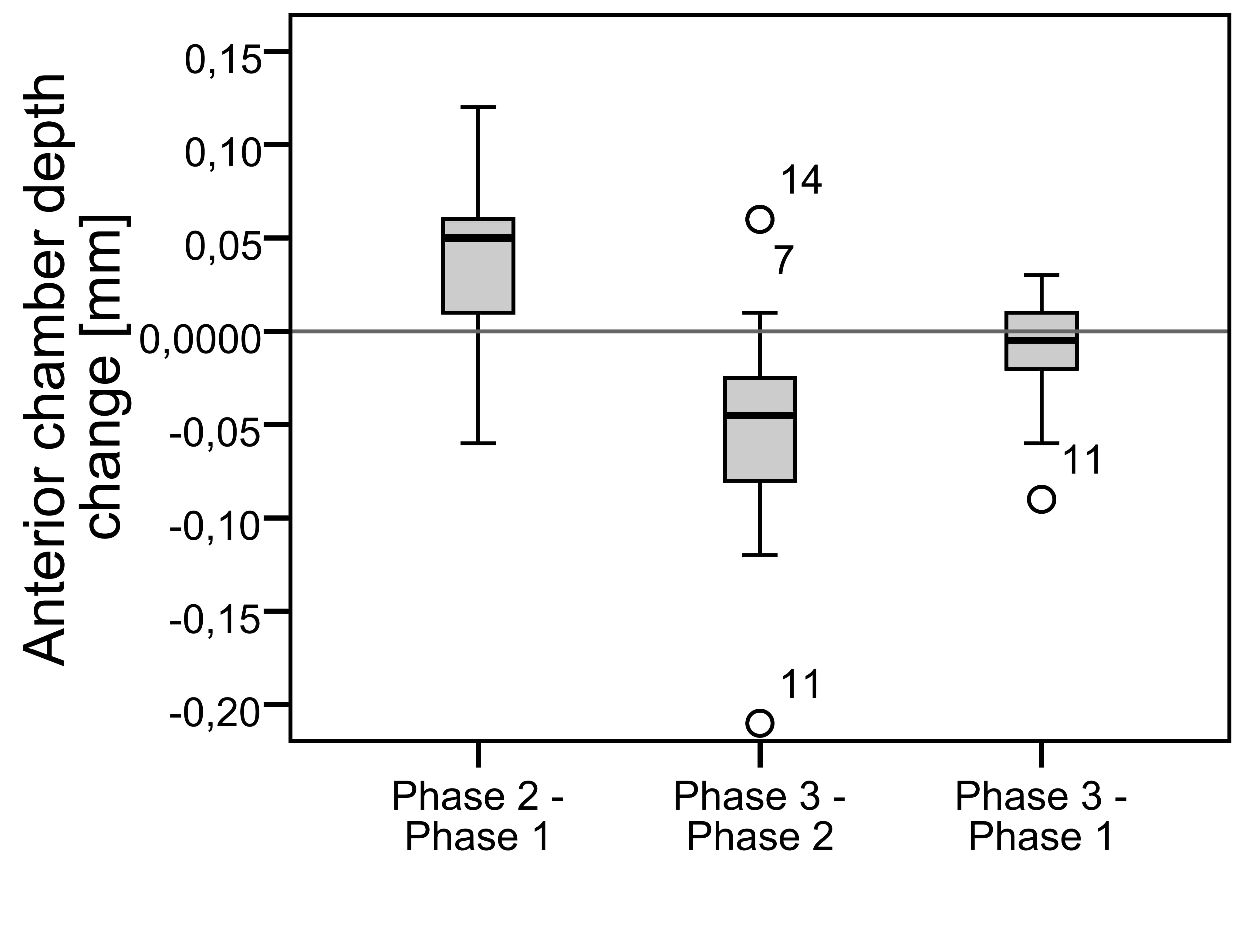
Results: No significant change in subfoveal CHT was found. The CHT decreased significantly only 1 and 1.5 mm nasally after discontinuation (-12 ± 21 µm p = 0.035 and -13 ± 17 µm p = 0.006) and increased 0.5 mm temporally after resuming the lens wear (+11 ± 17 µm p = 0.025). Both CCT and ACD increased significantly after discontinuation of ortho-k lens wear (+8 ± 11.0 µm p = 0.01 and +0.04 ± 0.05 mm p = 0.005) and then decreased again after resuming ortho-k lens wear (-7 ± 11 µm p = 0.03 and -0.05 ± 0.07 mm p = 0.009). AL did not change significantly between any of the study phases and correlated significantly negatively with CHT, but with no other parameters.
Conclusion: Subfoveal CHT did not change significantly due to short-term ortho-k lens treatment in adults. AL was not affected by the treatment either, despite the increase in ACD after discontinuation. Thus, ortho-k does not seem to have a short-term influence on AL.
Introduction
Changes in choroidal thickness (CHT) and corneal flattening are often mentioned as factors that could affect the validity of axial length (AL) measurements in myopia management when orthokeratology is used.1, 2 Furthermore, changes in CHT are commonly discussed as a possible reason for why orthokeratology treatment slows progression.3-5 The development of optical coherence tomography (OCT) provides a way for visualizing the choroid, so CHT and its changes can now be analysed. This is important not only in myopia control but also in retinal diseases because the choroid is important for the nutrition of the retina. Previous studies found that CHT correlates negatively with myopic refractive error, axial length, whereas the best correlation is with age.6-9 The choroid is thickest under the fovea with a decrease in the nasal part towards the optic disc.6, 7 Read et al10 found a significantly thinner choroid in myopic children aged 10 to 15 years compared to emmetropic children of the same age. CHT correlated also negatively with AL and refractive error, but positively with age. Zengin et al11 found a significant increase in CHT between 16 and 23 years, but no significant change in CHT between 4 and 16 years. Li et al in 20173 and 20194 observed changes in subfoveal CHT caused by ortho-k lens treatment in children. CHT increased significantly after one month of treatment; then there was only a small change after one year. One month after discontinuation of the treatment, the thickness decreased and was not significantly different from the baseline. In the control group (single vision spectacles) there was a significant decrease (mean 9 µm) after one year. The increase in CHT caused by ortho-k lens treatment was further reported by Jin et al.5 and Chen et al.12 Both Li3, 4 and Jin5 observed children aged 9-14 years, Chen12 7-17 years. Different results were published by Gardner et al.13 After 3 months, a significant decrease in 30 degrees superior and an increase in 30 degrees nasally were found, but there was no significant change subfoveally. However, only 9 children were included in that study.
A decrease in central corneal thickness (CCT) and anterior chamber depth (ACD) was reported after one month of treatment in the study by Li et al.3, 4 Age and change in subfoveal CHT after one month were associated with the AL change after one year of ortho-k lens wear. AL increased significantly. Conversely, Cheung and Cho2 did not find a significant difference in ACD in children after 6 months of orthokeratology treatment. In the control group, ACD increased significantly. However, considering the entire anterior segment (cornea to lens), there was no significant change in both groups. Therefore, according to Cheung and Cho2, the AL measurement is valid to monitor myopia progression. Similarly, Jin et al.5 reported a significant decrease in CCT and no change in ACD or AL after 3 months of treatment. The AL change correlated negatively with the CHT change. To conclude, the results of the previous studies are not in agreement with each other and no study about the changes in CHT due to ortho-k in adults was found. Therefore, the purpose of the current study is to investigate the CHT changes in adult ortho-k lens wearers after they discontinue and then resume ortho-k lens wear. Furthermore, measurements were taken to establish whether or not a potential change has an influence on AL or if AL is affected through the change in CCT or ACD.
Material and Methods
For the present study 16 eyes of 16 adult ortho-k lens wearers were included. Before this study was started, subjects had already been wearing lenses of reverse-geometry design (Falco Linsen AG, Switzerland and MPG&E, Germany). The duration of ortho-k lens treatment before the study ranged between 0.5 and 16 years (mean of 6.4 years). The mean spherical equivalent for the subject group (before they had started wearing ortho-k lenses) had been -2.5 D (range -0.5 to -4.5 D) with a cylinder not higher than 2.25 D. All subjects had reached a best corrected visual acuity of better than 20/20. Eight right and eight left eyes were randomly chosen. The subjects were between 25 and 54 years old, the mean age was 38. The study was carried out based on the revised Declaration of Helsinki 14, the regulations of Berliner Hochschule für Technik on ethics and data protection and the relevant legal requirements. Informed consent was obtained from every subject. Measurements were made in three study phases. The first measurement was taken after a minimum of six months of ortho-k lens wear. The lenses were worn regularly until the first measurements. The subjects were then asked not to wear their lenses until the second measurement that took place after approximately 4 weeks (range 23 to 34 days) when no more changes in corneal topography were to be expected. In this wash-out phase, spectacles or soft contact lenses were worn. However, the soft contact lenses were not worn at least 24 hours before the second term. The third measurement was taken after about 3 weeks (range 14 to 29 days) after returning to ortho-k lens wear. CHT, AL, ACD, CCT, refractive error, and visual acuity were measured for each study phase.
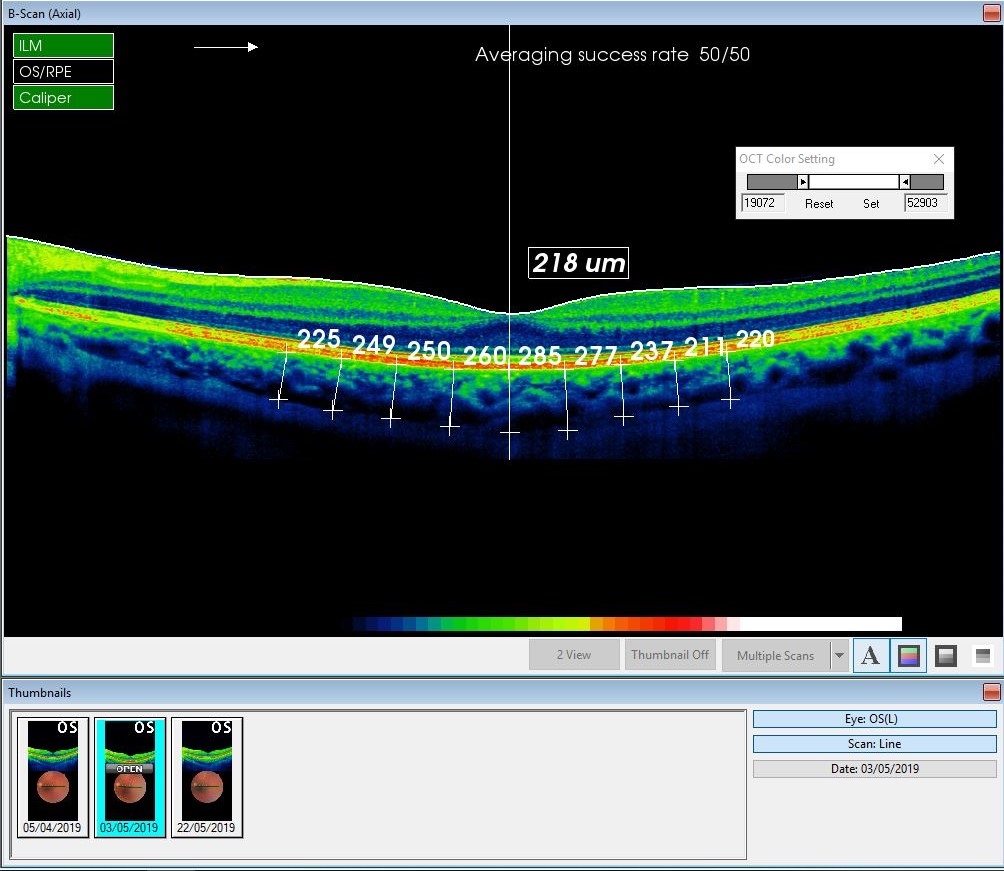
To measure CHT, a SD-OCT 3D 2000 (Topcon, Japan) was used. All scans were made using a 6 mm line scan, choroidal mode, using the instrument’s eye tracking function. The thickness was measured manually using a measurement tool of the Topcon software at nine locations - subfoveally (SF) and 500 (T0.5), 1000 (T1), 1500 (T1.5), 2000 µm (T2) temporally and nasally (N0.5, N1, N1.5, N2) from the fovea. The thickness was defined as the distance from the posterior edge of the retinal pigment epithelium to the junction between the choroid and the sclera (Figure 1). A Pentacam AXL (Oculus Optikgeräte GmbH, Germany) was used to measure AL, ACD, and CCT. All measurements were made between 2 and 6 pm to minimize the potential influence of diurnal variation. The analysis was made with the software IBM SPSS Statistic Version 24 and Microsoft Excel 2013. In the descriptive statistic mean differences between 1st and 2nd, 2nd and 3rd and 1st and 3rd measurements, standard deviations and ranges were calculated. Pearson correlation was used to determinate if there is a linear relationship between the changes in AL and CCT, ACD and subfoveal CHT. For the inductive statistics, the following null hypothesis was determined: Orthokeratology has no short-term influence on AL, CCT, ACD and CHT. The normal distribution was determined with Kolmogorov-Smirnov Test and Shapiro-Wilk Test. Alpha was defined as 0,05 and the 2-tailed significance was used. Evaluation whether the difference between the measurements is significant, and whether the null hypothesis can be rejected, was made with Paired t-test and additionally with the Wilcoxon signed ranks test for values that did not show the normal distribution in some of the tests for normality.
Results
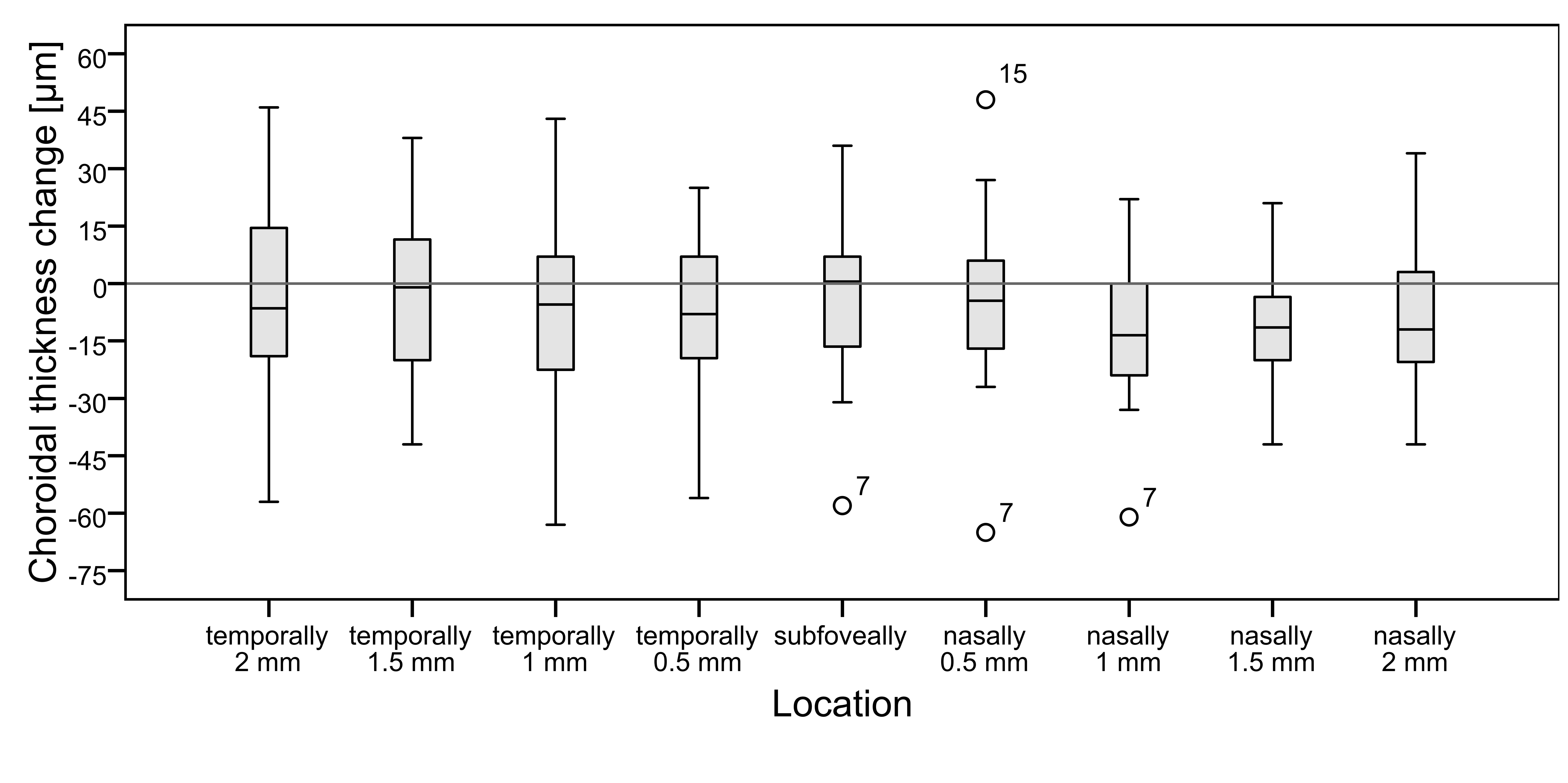
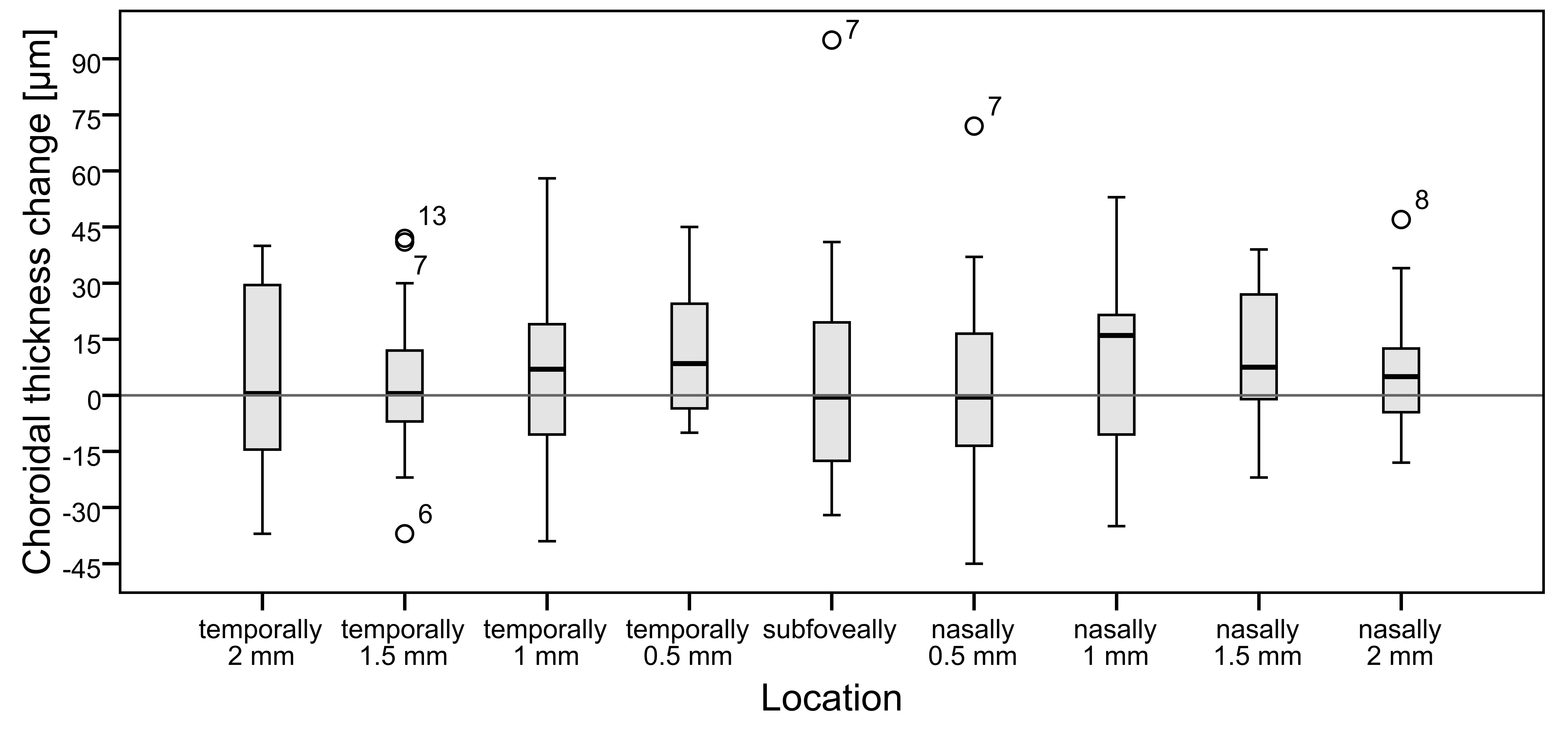
Choroidal thickness
Subfoveal CHT ranged between 211 µm and 545 µm with a mean ± SD of 345 ± 97 µm after orthokeratology treatment, 230 µm to 559 µm with a mean ± SD of 341 ± 103 µm after discontinuation, and 206 to 581 µm with a mean ± SD of 347 ± 100 µm 2 to 4 weeks after resuming the treatment. The measurements of the three study phases were then compared. The mean value of CHT decreased after the discontinuation of the treatment in all regions and increased again after resuming lens wear. However, there was a noticeable variation within the data, and in some subjects, even the opposite change was found. The change in CHT was significant after the discontinuation only at 1 mm (N1) and 1.5 mm nasally (N1.5) (mean of -12 ± 21 µm p=0.035 and -13 ± 17 µm p=0.006 respectively). There was no significant change in the subfoveal part (-4 ± 23 µm p=0.5) (Figure 2). Two subjects were considered outliers (at SF and N1 subject 7 and at N0.5 subject 7 and 15). Excluding the outlier subject 7 at 1 mm nasally, no more significant change was found (-9 ± 17 µm p = 0.063). There was no change in the insignificance of the results subfoveally (p=0.98) and 0.5 mm nasally (p=0.32) when excluding the outliers.After resuming ortho-k lens wear, CHT increased significantly in 0.5 mm temporally (T0.5) from the fovea (mean of +11 ± 17 µm p=0.025). Again, the subfoveal part did not change significantly (+5 ± 31 µm p=0.5) (Figure 3). There was no significant change of CHT between the first and the third study phase (both times during the treatment). However, the range of changes was quite large (-59 µm to +54 µm).
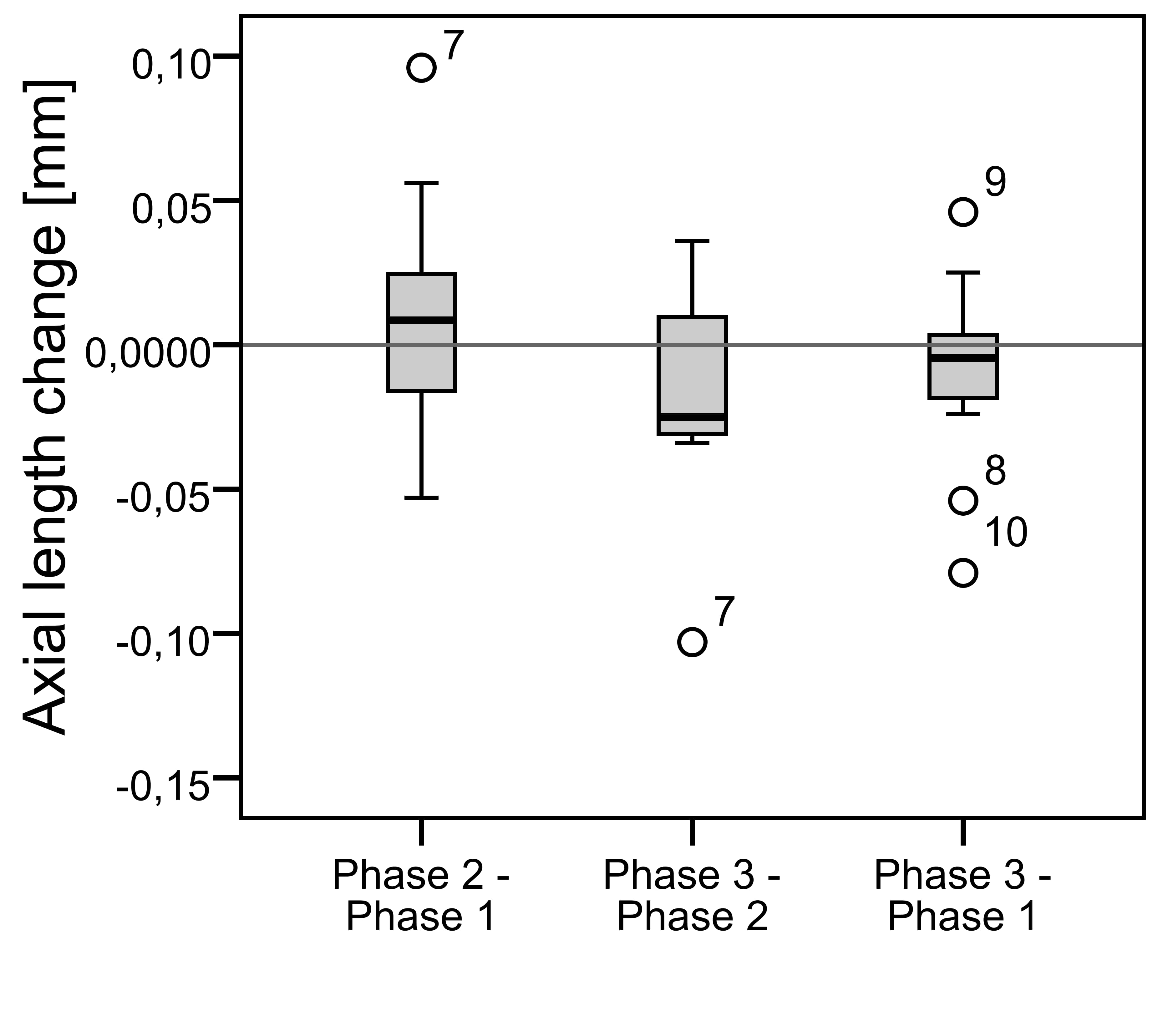
Axial length
Mean AL ranged between 23.5 and 25.4 mm in all three study phases and did not change significantly between either of them (Figure 4). The mean change in AL was +0.008 ± 0.037 mm p=0.5 after the discontinuation (implying a non-significant increase in AL) and -0.016 ± 0.033 mm p=0.07 after resuming treatment (implying a non-significant decrease in AL).
Central corneal thickness and anterior chamber depth
CCT and ACD increased significantly after the discontinuation (mean ± SD of +8 ± 11 µm p = 0.01 and +0.04 ± 0.05 mm p = 0.005 respectively) and decreased significantly after resuming lens wear (-7 ± 11 µm p = 0.03 and -0.05 ± 0.07 mm p = 0.009 respectively). There were no significant differences between the first and the third term (for CCT p=0.36 and ACD p=0.16). The mean of CCT and ACD after the discontinuation of the lens wear was 531 ± 32 µm and 3.03 ± 0.33 mm respectively (Figure 5, Figure 6).
Correlation between the parameters
The change in AL after the discontinuation of lens wear correlated best with the change in subfoveal CHT. There was a significant negative correlation (-0.68 p=0.004). This means that when AL decreased, the subfoveal CHT increased. There was a nonsignificant weak positive correlation between the change in AL after the discontinuation of ortho-k lens wear and the change in CCT and ACD. Similarly, after resuming lens wear only the CHT change correlated significantly negatively with the AL change (-0.65 p=0.007).
.
.
Discussion
Choroidal thickness
CHT changed significantly only in a few peripheral regions but not subfoveally. Previous studies have used a different design. They measured before the start and after a certain time of the ortho-k treatment and the subjects were children. In the present study, a reversed study order had to be used because the study group consisted exclusively of existing adult ortho-k lens wearers, and no pre-wear-data regarding the parameters of AL, CHT etc. existed. Gardner et al.13 found similarly to this study no significant subfoveal change. In contrast, Li et al.3 and Jin et al.4 found a significant change of subfoveal CHT (mean ± SD of +16 ± 11 µm and +9.8 ± 23.5 µm respectively), the change was measured after 1 month of ortho-k lens wear. Chen et al.12 found a significant increase of +21.8 ± 25.2 µm in the parafoveal region. That is the biggest change from the listed studies. They also measured children, however, in the morning. The diurnal variation could also cause different changes. To compare, this study found that subfoveally the mean change was only -4 ± 23 µm (Table 1). It should be considered that all mentioned studies were conducted in children, the current study in adults. Because different studies reported a decrease in CHT with age6, 7, it could be expected that in the thinner adult choroid the change will be smaller. This could also explain the different results of Gardner et al.13, as he observed older children in his study. The findings of the current study do not support this explanation, as the Pearson’s correlation analysis did not show a significant correlation between the change in CHT and age. However, a negative correlation was previously reported by Michalewski et al.6 and Flores-Moreno et al.7 They used bigger samples (122 and 120 eyes) and their subject group had a higher age variability (age of subjects ranged from 15 to 79 years and from 5 to 99 years respectively). Thus, the previously shown correlation may not be strong enough to be significant in our small sample.
To minimize diurnal variation, this study and all the cited studies took the measurements at the same daytime period, with the exception of Gardner et al.13 They made only 32/45 measurements in the afternoon and the exact time is not stated.
The reason for the different results of the present study when compared to other studies regarding the changes in CHT might also be due to the small sample size, because with a small number of subjects, it might be more difficult to find significance in small changes. Another reason for our results and for a large SD could be seen in the different duration of the ortho-k lens treatment before the study (0.5 to 16 years). The vision of all participants was already stabilized before the first measurement, so it can be expected that the CHT stayed the same over the time, although we have no data to prove this assumption.
Central corneal thickness
CCT increased significantly after the lens wear discontinuation (mean ± SD of +8 ± 11 µm) and significantly decreased again after resuming ortho-k lens wear. This confirms the results of previous studies made by Li et al.3, Jin et al.5, and Cheung and Cho2. They found a significant change in CCT of -12 ± 7 µm, -6.3 ± 7 µm, and -9 ± 9 µm respectively (Table 1). The results are also in agreement with the hypothesis that ortho-k lenses correct refractive error through flattening of the central corneal surface concurrent with a decrease in CCT.15-18
Anterior chamber depth
In contrast to the current study, ACD did not change in the studies presented by Jin et al.5 and Cheung and Cho2 (Table 1). It should be noted that they measured changes in children and after a longer time period. Thus, the eye growth could affect the results. The hypothesis of eye growth as a confounding factor is supported by the fact that Cheung and Cho2 measured a significant increase in ACD in the control group. The results of the current study then pose the question of how ortho-k lenses can influence ACD. The eye growth or age-related changes cannot be the reason, because although the ACD increased after the discontinuation of ortho-k lens wear, ACD decreased again after resuming lens wear so that there was no significant difference between the first and the third measurement."
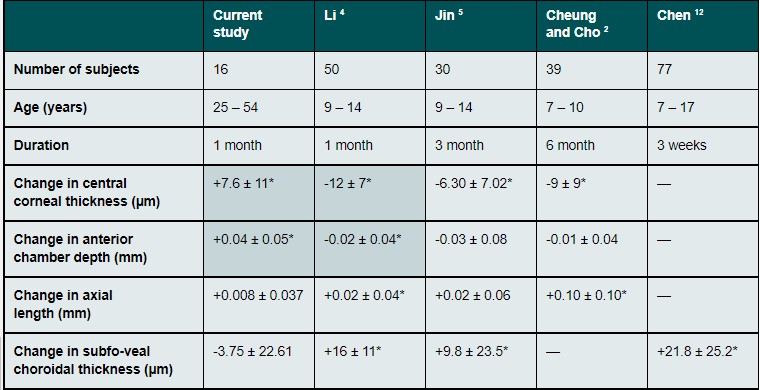
Axial length
Since no significant change in AL was detected between the three phases of our study, we can assume that there is no short-term effect of ortho-k lens treatment on AL. Thus, AL seems to be a reliable factor to monitor the progression of myopia, no matter whether ortho-k is used or not. However, it should be emphasized that no significant change in AL was found despite the changes in ACD and CCT. These parameters are constituents of the AL. The current study also did not find a significant Pearson correlation of AL and CCT or ACD. The reason for finding no significant change in AL despite the significant change in ACD may be, again, the small number of subjects or that, in comparison, small variations within numerically larger (longer) parameters, such as AL, are more difficult to find than small changes in numerically small (shorter) parameters of the anterior segment. Comparison with other studies is difficult. Li et al.3 and Cheung and Cho2 found a significant increase in AL after starting ortho-k lens wear. Jin et al5 found an increase, too, but it was not significant (Table 1). Their findings are the exact opposite of the speculation that ortho-k lenses might cause a decrease in AL. However, the three studies were conducted in children, over a time period of 1, 3, and 6 months (Li et al.3, Jin et al.5, and Cheung and Cho2 respectively), where eye growth is to be expected. The growth could outweigh the decrease due to ortho-k lens treatment. Because AL was measured only to the pigment epithelium of the retina, the change in CHT could have had an additional influence. If the choroid decreases after discontinuation of ortho-k lens wear from the inner side, it would cause an increase in AL and so add to the change in the anterior segment. In that case, it could not cause the nonsignificant change in AL of the present study. However, the current study did not find a significant change in the subfoveal choroid, therefore it could not be a reason for the non-significant change in AL.
Conclusions
This study investigated changes in AL, CCT, ACD, and CHT one month after the discontinuation of ortho-k lens treatment (in the duration of 0.5 to 16 years) and after 2 – 4 weeks of resuming ortho-k lens wear in 16 adult subjects. The subfoveal CHT did not change significantly after the discontinuation of ortho-k lens treatment or after resuming lens wear.
Therefore, there was no short-term effect of ortho-k lens treatment on the subfoveal CHT. After the discontinuation of ortho-k lens wear, CCT and ACD increased significantly. Despite this, there was no significant change in AL, so there was no short-term effect of the treatment on this parameter. This suggests, that measurement of AL is a valid factor to estimate the efficacy of ortho-k lens treatment in myopia management.
Studies with larger sample sizes are required to verify this finding, and to investigate the changes in CHT in adults and their relationship to myopia progression. Furthermore, the reason for the significant change in ACD in the absence of a simultaneous significant change in AL remains unclear.
Conflict of Interests
The authors declare that there is no conflict of interests regarding the methods and devices mentioned in this article.
COE Multiple Choice Questionnaire
The publication "Short-term effect of Ortho-K on axial length and choroidal thickness" has been approved as a COE continuing education article by the German Quality Association for Optometric Services (GOL). The deadline to answer the questions is 01. July 2023. Only one answer per question is correct. Successful completion requires answering four of the six questions.
You can take the continuing education exam while logged in.
Users who are not yet logged in can register for ocl-online free of charge here.
