Method(s) and application of visual training in practice for patients with central visual field defects
Purpose: The aim of this clinical study is to discuss eccentric viewing training for patients with central visual field defects.
Material and Methods: In order to improve the usability of optical or electronic magnifying aids and to regain reading skills, eccentric viewing training may be necessary in patients with central scotoma. Based on the visual training of Nilsson et al.1, we carried out a training with two rehabilitees at the Regiomed Rehabilitation Clinic Masserberg using simple self-made aids (optical magnification by means of overaddition and illuminated magnifying glasses; prepared exercise sheets with different texts / font sizes). We were able to find an area below the lesion that can be used for reading using letters of different sizes, which are pushed from the periphery in the direction of the visual centre. Within this area, the moving test letter can be read permanently. The subsequent attentional training sensitises the patient to the usefulness of this area, where text samples of different sizes are subsequently presented.
These were then read aloud with appropriate close correction / enlargement (observing the working distance) (moving text = moving text with steady eye = unmoving eye).
Results: One rehabilitation patient already benefited so much from the use of the newly adapted magnifying aids, that additional visual training showed no clear additional benefit. The other rehabilitation patient could not overcome the hurdle of the small working distance, despite intensive motivation, so that no success due to the training could be determined.
Conclusion: Although the small sample cannot show direct success, it can be stated that eccentric viewing training can work without complex technology. Application to a larger population should be pursued. For more variations and fast, individual adaptation, the use of special software seems desirable.
Introduction
Due to central scotomas, affected individuals notice an increasing loss of detail vision and central blurring, which make reading difficult or almost impossible. Besides age-related macular degeneration (AMD), other maculopathies (e. g., central serous retinopathy, macular oedema) or neurodegenerative diseases (e. g., cone dystrophy, neuritis nervi optici) may result in central scotomas.
For patients who are considered to be untreatable, the perceived deficits due to the visual impairment lead to a loss of quality of life (QoL)2, especially with increasing age. For this reason, referral to continuing rehabilitation services is critical.3 These include low vision specialists or special outpatient clinics at university eye clinics for visual impairment or inpatient rehabilitation facilities, such as the Regiomed rehabilitation clinic in Masserberg, which offer strategies to compensate for the visual deficit, for example.
In addition to fitting magnifying aids, it is possible to compensate for one’s deficit by means of special compensatory reading or visual training.
Reading: prerequisites and determining reading speed
Reading requires a sufficiently high central visual acuity (newspaper print at 25 cm: visual acuity 0.4) and a sufficiently large reading visual field. This extends to a minimum of 2° to the right and left of the fixation point and thus corresponds approximately to the size of the recognisable letter area of the fovea.4 With parafoveal information acquisition, the perceptual area extends asymmetrically further up to 5° (or 15 letters) in the reading direction.
Reading as a complex skill requires not only visual processing but also oculomotor control and subsequent cognitive processing. Reading is characterised by a sequence of saccades whose goal is to keep the letters in the foveal region and thus enable recognition at the location of maximum visual performance. Forward saccades describe a movement of the eyes along the line of text, backward saccades proceed in the opposite direction. Such saccades are associated with text processing difficulties. At the end of the text line, a long backward saccade toward the beginning of the next line becomes necessary.
Depending on the examination task, the use of special reading tests is recommended. Due to better consistency and reproducibility, especially for repeated measures and progress controls (after / during an intervention5), the longer paragraphs of the International Reading Speed Text (IReST)6 are better suited for simulating real-life reading than the single-sentence utterances of the Radner Reading Tables.5,7 Single-sentence tests allow rapid testing for possible reading disorders in clinical practice. The use of randomised reading charts allows conclusions to be drawn about real reading performance, since subsequent words cannot be anticipated but must actually be recognised.8
Reading and reading speed (in central scotoma): influencing factors
Factors which influence reading speed include:
- Age: decrease in reading speed by approx. 20 % comparing a group of 18 – 35 year-olds to 60 – 85 year-old test subjects.6,9
- Crowding:10–13 Decrease in reading speed due to fusion of features over an inappropriately large area as the fixation moves away from the target.
- Decrease of the visual span towards the periphery: fewer letters can be recognized simultaneously without interference.14
- Text characteristics: sentence structure, level of difficulty, associated with the frequency of occurring words,15 linguistic complexity,16 and logical context of the sentence.17
- Reader interest in the text.
Due to the central loss of vision in patients with AMD, a peripheral retinal locus (next to the lesion) has to be used: the so-called PRL (preferred retinal locus, also “pseudo-fovea”; in healthy eyes = fovea). Due to spontaneous, partly unconscious formation, a self-selected PRL may not be ideally localised.18 Often PRLs are chosen left of the central scotoma, possibly because of the habitual reading direction (left to right) in western countries,19 which, however, causes the scotoma to cover the text in the direction of reading. Mackeben et al.20 find that a more right / left scotoma leads to an omission of letters at the end / beginning of words. Because they cover the reading text the least, PRLs below or above the scotoma (above / below the lesion) seem ideal,21 although studies do not all agree due to the sum of influencing factors.18 Patients with juvenile macular degeneration (e. g., Mb. Stargardt) already increasingly use a PRL below the scotoma,22 whereas older AMD patients use a PRL to the left of the scotoma.23 Moreover, different PRLs may develop for different tasks, for example recognition of single letters (visual acuity testing) versus word recognition in reading, also under different contrast and illumination conditions.24 In addition to the location of the PRL, other factors influencing reading speed in AMD are discussed:18,21
• Decrease in visual span in peripheral areas, associated with slower processing of letters and words compared to individuals with “normal” periphery and reduced saccade planning.
• Reduced oculomotor control: foveal saccades are easier to perform than “non-foveal” saccades.
• Reduced forward saccades, increased backward saccades (assumption: shorter paragraphs / sentences read faster because they require fewer reset saccades to the beginning of the line, especially if the beginning of the line does not fall within the scotoma).7
• Suspicion of influences of fixation (in)stability (not clearly detectable).25
• Font: Radner Reading Table (Arial) possibly more difficult to read than IReST (Times New Roman).26
• Magnification requirement (MR): the more peripheral the PRL, the higher the MR,4,27 and the lower the reading speed.28
• Influence of fatigue (hypothesis): increased effort required to plan and execute saccades, which is why longer texts are more tiring to read than single-word / single-sentence utterances.7
Rehabilitation: compensation options
Magnifying aids compensate for the visual deficit in central scotomas and are associated with improved reading speed, cognitive status and quality of life.7,28–30 It is advisable to combine the provision of assistive devices with additional (eccentric) reading or vision training for further improvement of reading speed and a more relaxed use of magnifying devices.3,28,31
The following training methods can be distinguished, but are not completely independent of each other:
- eccentric vision training;
- controlled eye movements; and
- attentional training.
Eccentric vision training
During eccentric vision training, patients learn to use a new eccentric retinal locus for fixation. If the usual PRL is not available or not ideal, the patient is trained to use a more suitable retinal location, the TRL (trained retinal locus). In perimetry, a shift of the blind spot as a reference scotoma provides information about an already existing eccentric visual position (e. g., upward / downward in comparison to normal on the horizontal axis). One of the goals of TRL training is to raise awareness of this new location. As an illustration for the patient, the therapist (e. g., optometrist, orthoptist, occupational therapist) can hold their own hands R / L from their head, with the nose forming the centre and accordingly not being seen by the patient sitting opposite. The principle of eccentric vision is explained when the therapist moves their hands upwards until the patient can see the nose.
One possibility of eccentric vision training is performed in 4 steps 23 partly under control of a scanning laser ophthalmoscope (SLO). By using an SLO, the displacement of the lesion can be observed (fundus observation) simultaneously to an eye movement (e. g., fixation stimulus in the context of eccentric vision training). This allows a precise and later, for the patient and therapist, clear training, but is not mandatory. First, the eccentricity with which an enlarged letter, initially invisible and projected centrally onto the retina can be recognised (large cross (“+”); the patient fixates on the centre of the cross; this is followed by a movement of the horizontal axis upwards, the gaze follows (= fixation on centre of the cross) until the letter becomes visible; parallel observation of the lesion via SLO; moves downward). In comparison, Seiple et al.32 use the representation of a clock with a central star and peripherally located numbers (size 1.7°) to determine a suitable retinal location. The scotoma is successfully shifted toward / onto the respective number using directed eye movements; thus, it can be determined where the central star is most distinct and, consequently, the best possible eccentric gaze position can be found. For asymmetric scotomas, Nilsson et al.23 additionally check the downward gaze to see if a more suitable retinal location is found here (lower eccentricity, higher visual acuity). The necessary letter size at the corresponding retinal location provides information about the possible, usable visual acuity. For easier reading, a magnification slightly above the determined magnification requirement is used. Subsequently, the patients have to read aloud a text magnified 8 – 15 times, slowly scrolled at the beginning, which is presented on this new retinal location. The SLO allows for ongoing instruction and correction. Following SLO training, monocular hyperocular lenses (10 – 15x magnification; 40 – 60 D)1 are mounted in a spectacle frame and the opposite eye is occluded. Due to the now uncomfortably reduced reading distance (2.5 cm – 1.7 cm), high motivation by the therapist(s) is required for the patient to read the text aloud nevertheless. Additional guiding lines are inserted above or below the text to help locate fixation stably at the eccentric position. As other strategies for eccentric visual training,18 this method works with a moving text through the TRL, while keeping the eyes as steady as possible. As the training progresses, the guides are removed. The weekly training sessions in the clinic last one hour. In the time to the next appointment the patients should practice at home. On average, after 5 – 6 hours of training, 90 % (18 / 20) of the test subjects (TS) showed an improvement in reading speed from 9 ± 5.8 wpm (words per minute) at baseline to 68.3 ± 19.4 wpm, which remained stable after one year. 12 of the TS chose a location above, 6 below the lesion with an average of 7.8° ± 2.0° of the required deflection (range: 5 – 12°) and an average magnification requirement of 14.3-fold. The better the initial conditions were, the younger the patients, the better they were already able to read even with the usual use of aids, the faster and to a greater extent training successes were shown. We trained two TS using this methodology at the Regiomed rehabilitation clinic in Masserberg (see case studies).
Controlled eye movements
In the past, attempts were made to use acoustic signals to bring the eyes rhythmically and precisely to the desired fixation location or to keep them there (= biofeedback, e. g. microperimeter MP-1 from Nidek).33 The increase or decrease of the pitch or the continuity of the tone helped the patients to train their awareness of their own eye movements. The goal is to achieve an increased fixation stability or an easy reference to the PRL. A sound signal when approaching the PRL showed the greatest effect.18 In comparison, also by means of different dot and letter schemes (variation of distance and number), an improvement of the reading speed of the AMD patients (54 – 89 years; median 79) by 27 ± 3 wpm was achieved.32 Additional sensorimotor training of patients with juvenile macular degeneration using a window moving from left to right, which contained a defined portion of text, also resulted in an increase of reading speed by 20 wpm (median).21 Overall, it can be assumed that eye movements and gaze positions can be trained.
Attentional training
Performance appears to be highest at the site of central attention (in ocular health = often the site to which the visual centre is directed), and there is improved or stronger perception of stimulus properties at this site.34 By means of attentional training, attention is consciously directed to stimuli in the periphery, which significantly increases reading speed.18,31
Rapid serial visual processing (RSVP) can also be understood as attentional training. In a randomised controlled trial, under SLO control, an eccentric fixation cross was projected onto the retina at the location of the PRL (usually in the area 6° radius above the lesion).28 Then, a sequence of magnified single words was presented rapidly at this position (RSVP). Subjects were instructed to keep their gaze position stably aligned with the cross while reading the words aloud. For the (home) training (6 weeks, 5 days / week for 30 minutes each) with the training laptop we chose the magnification at which reading comfort could be maintained. The same magnification requirement was maintained for reading the IReST charts during the follow-up appointments in the clinic. A median increase in reading speed of 14.7 wpm was noted (74 wpm to 88.7 wpm), which remained stable after 6 weeks without training (90 wpm). Overall, 38 % (14 / 37 TS) improved their reading speed by at least 10 wpm. Although the RSVP does not allow reading saccades and does not allow reset saccades, a transferability of the training successes of the RSVP to “real” reading is evident by the increase in reading speed when reading the IReST panels during the clinical control examinations. Besides, we also observed a positive effect on the emotional state and the perceived quality of life of the patients.
With increasing age, the cause of a lack of training success 21,32 may be due to reduced neuronal plasticity.35 The strategies learned through RSVP can also be transferred to other eccentric positions or to the “untrained” eye and its effects are stable even after months.18,31
Case studies: eccentric vision training
At present, only limited training materials for eccentric vision training are available at the Regiomed rehabilitation clinic in Masserberg, which were created ad-hoc for this study based on the described literature. We used the text material of the IReST plates 1 – 8, in different font sizes (10 – 26), in the font Verdana (https://www.leserlich.info/). For the “moving text” at “steady eye”, the texts were printed on clear slides and, for the training at home, auxiliary lines were added above the text lines (picture documentation in preparation).
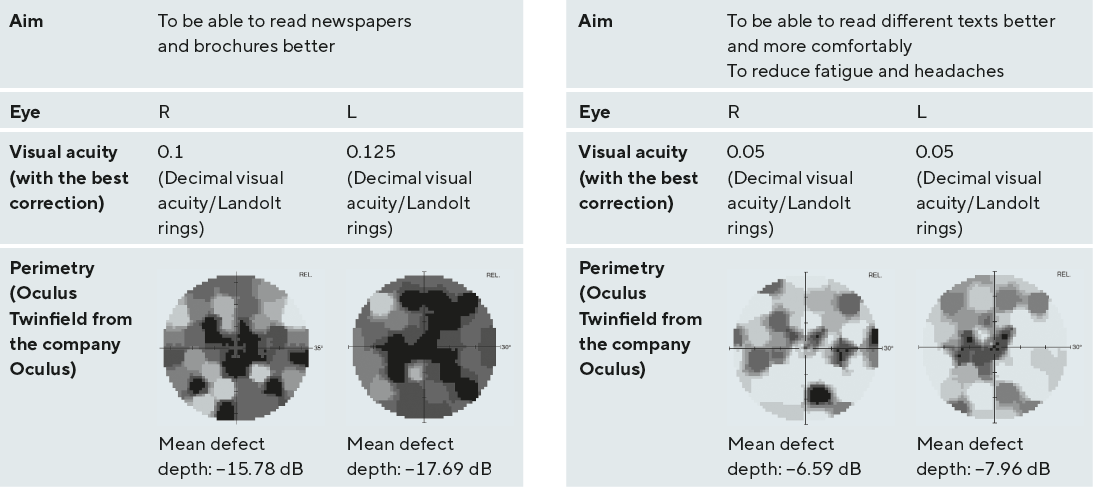
Two rehabilitation patients (Tables 1, 2) of the Regiomed rehabilitation clinic in Masserberg were chosen for the case study. Perimetry (Goldmann – test mark III4e; threshold determination with Heijl Krakau fixation control) showed a central scotoma in both eyes, with peripherally still sufficiently large horizontal areas. After subjective refraction, we could determine the eye more suitable for training. The eccentric visual training was performed monocularly, with best correction and adapted magnification (determination by means of reading samples of Eschenbach and Fa. Oculus). The training motivation was determined after a detailed anamnesis and questions about reading habits and wishes, such as what the TS would like to read again. The two rehabilitation patients were treated according to the ethical principles of the Regiomed rehabilitation clinic in Masserberg as well as the principles of the Declaration of Helsinki and had agreed to the training.
The procedure for eccentric visual training is illustrated by the case studies. Despite more pronounced central scotomas in TS 1 than in TS 2, better visual acuity values were determined. Based on perimetry, it could be seen that a PRL was not (yet) being used (no shift of the blind spot as reference scotoma). An empirical magnification requirement of at least 2.5x for newspaper printing, at a working distance of 25 cm (reading sample from Eschenbach) for TS 1 and at least a 6.25x magnification for TS 2 was determined (mathematically higher magnification required: TS 1 at least 4x, TS 2 at least 8x). A magnification above this magnification requirement should be used to maintain reading comfort while training.
Step 1: Determining the retinal area
The most suitable eccentric retinal area was determined after selecting the more suitable eye (TS 1: L / TS 2: R) for monocular training (occlusion of the opposite eye). For this purpose, a prepared rod with a letter was moved around a fixed mark (rhombus) and the locations where the letter could be recognised were marked. The letter size used provides a possible indication of the usable visual acuity (Figure 1). Ideally, a horizontal retinal area below the scotoma was used. During testing, the test subjects wore the usual near-correction aids at a subjectively comfortable working distance.
Step 2: Sensitise the retinal area
This step is used for attention training. The TS are further instructed to look at the fixed mark (rhombus) with their usual near correction aids while objects / groups of letters or numbers are presented in the identified area to be read aloud. The aim is to achieve a steady reading rhythm. The eye movements are observed at the same time. Once a regular rhythm and regular reading saccades have been achieved, we moved on to step 3.
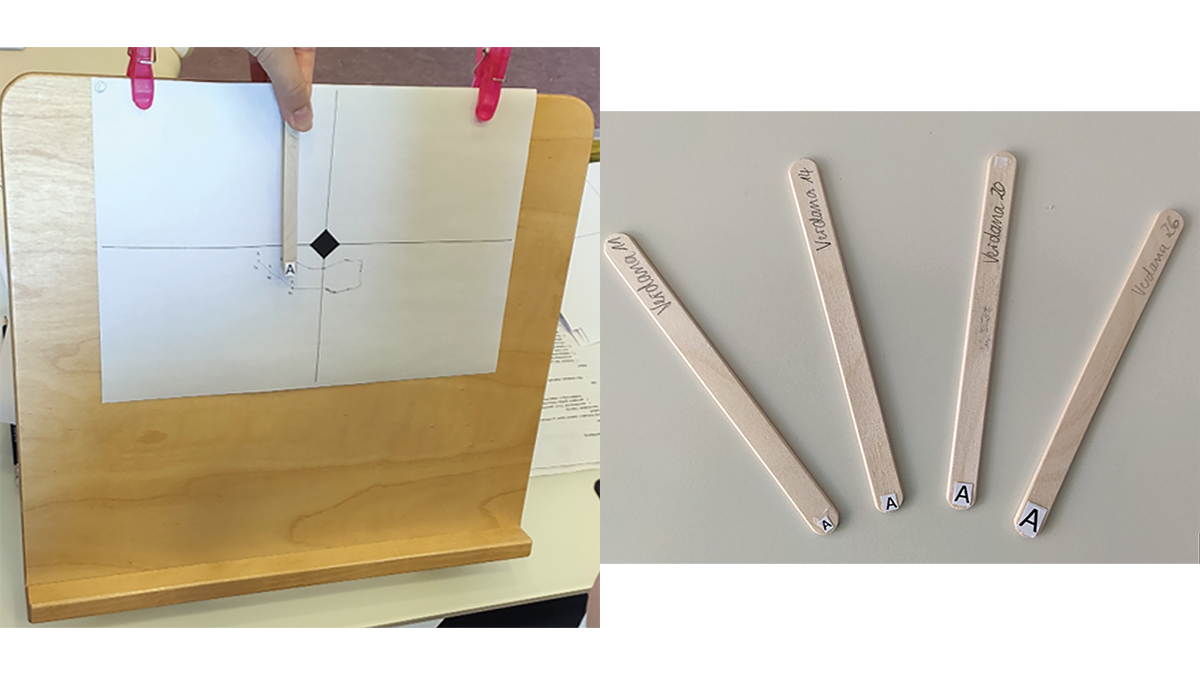
Step 3: Reading training
The TS continued to fixate the rhombus monocularly while a text was shone on the retinal area to be used (Figure 2). We started with large text sizes (e. g., Verdana 26), which were then reduced as the exercise progressed, with a simultaneous increase in optical magnification and reduction in working distance. Ideally, newspaper print can finally be read at an acceptable reading distance.
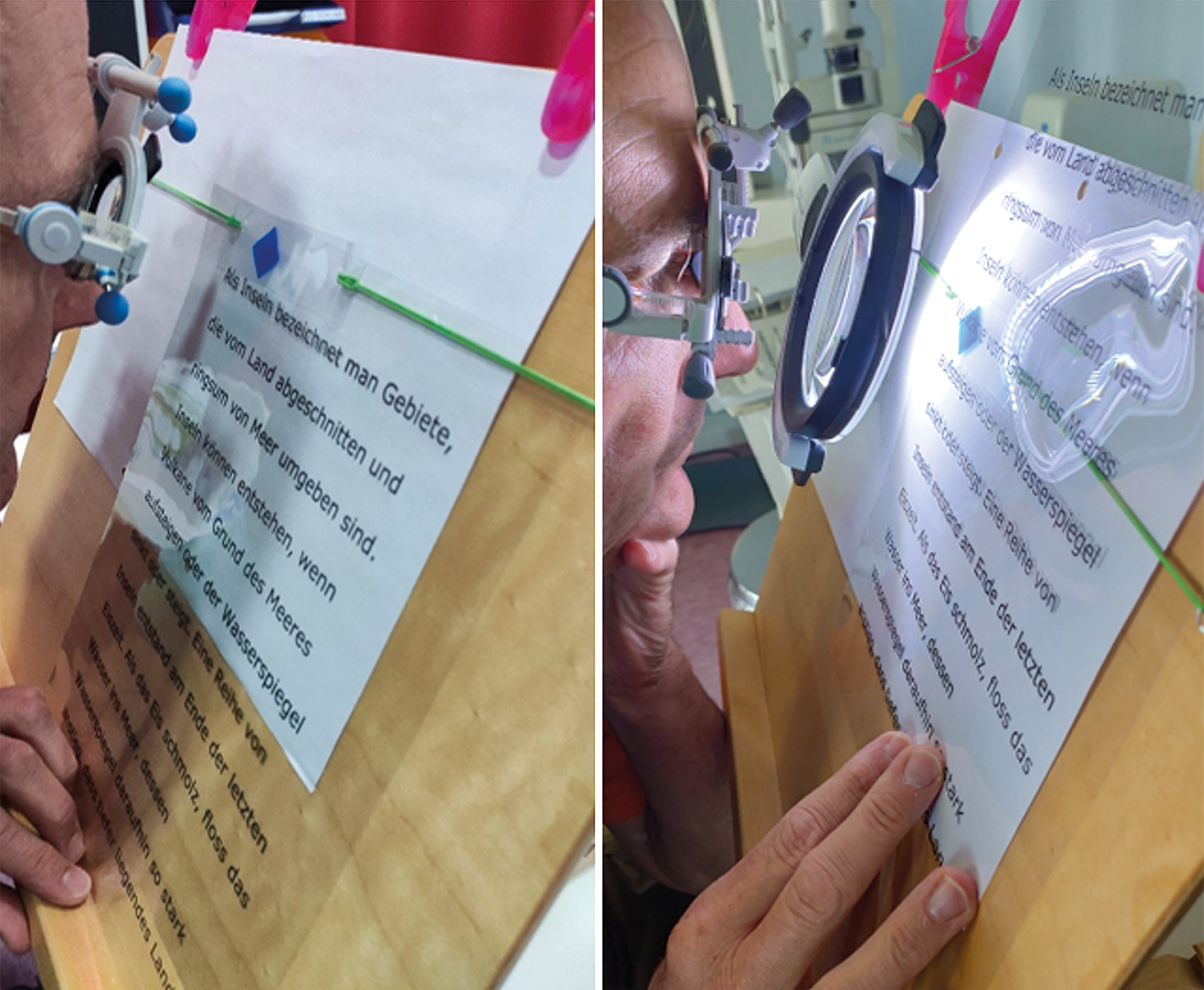
Within the clinical training, it was noticeable that TS 1 already used the available aids very successfully (reading glasses in combination with illuminated hand magnifier) and thus could already read font sizes of 14 / 16 points almost without problems. After a short time, even the smallest text size (font size 10) could be read at a comfortable working distance of approx. 30 – 35 cm (Figure 3). In comparison, TS 2 did not notice any significant improvement from the optical magnification (overaddition (between 10 – 16 D) in combination with the use of an illuminated bench-top magnifying glass of 2.5 D; note: font size / type Verdana 26), since the shortened working distance and the posture adopted were subjectively too unfamiliar and caused postural pain. Despite intensive motivation, persistent training was hardly possible.
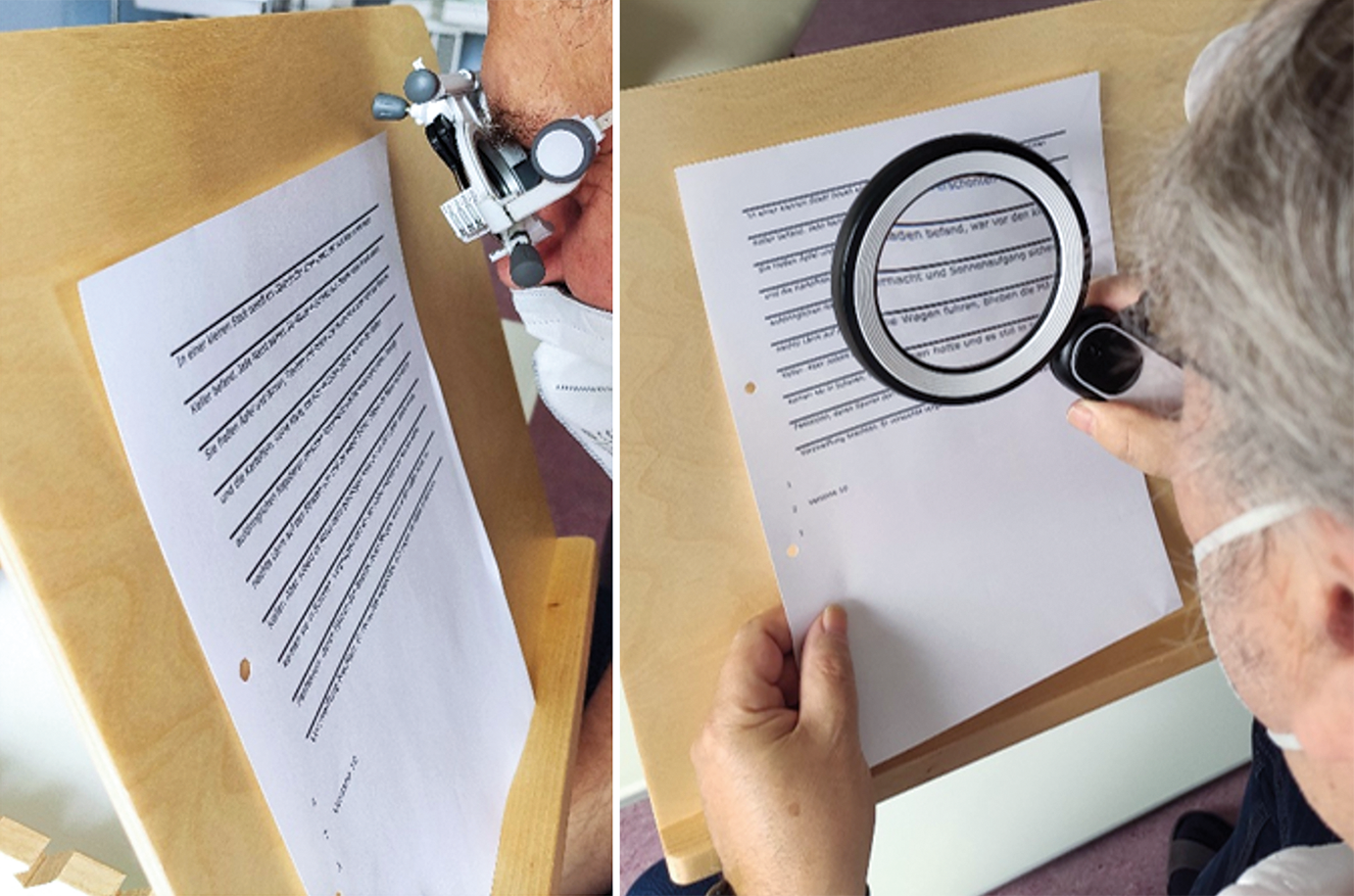
Step 4: Learning the “moving text” strategy
Finally, the TS practised independently sliding the text from right to left through the trained retinal area. A printed text on a solid surface (e. g., reading desk or clipboard) was used that could be clearly recognised with the determined near correction. Initially, the TS could use texts with an auxiliary line above or below the text line (Figure 4), which served as a guide for fixation. In the further course of training, these lines were removed.
Since TS 1 progressed rapidly, no further appointments were necessary. For further reinforcement, home practice sheets with different sized texts (IReST panels 1 – 8) including guiding lines were handed out. As the font size decreases, more words per line must be read (Figure 4). TS 2 underwent a total of 4 training sessions (60 minutes). As a result of the unfamiliar and painful posture as well as the rapid fatigue, only 30 minutes of these trainings were effectively used. Although subjectively hardly any improvements were noticeable, the reading speed increased from approx. 25 minutes for IReST board 8, font size 26 (approx. 5.2 wpm) to approx. 19 minutes (approx. 6.8 wpm). Thus, an improvement trend in reading speed is evident, although not clinically relevant. TS 2 also received home practice sheets, already at the beginning of training, but did not practise with them. Unfortunately, due to time constraints, no further practice sessions, including on the screen reader, could take place. It remains questionable to what extent the few practice sessions were sufficient to learn to exploit the eccentric retinal site. The indifference towards training at home points to a lack of motivation.
Discussion
In central scotomas, low vision care with magnifying aids is the method of choice and achieves the greatest possible effect in improving reading speed, which can, however, be further supported by additional reading or vision training.28 An increase in visual acuity is neither expected nor achieved by the use of aids, nor by training. However, it could be shown that a 4 – 5 hour training with aids for a screen reader can achieve a stable improvement in the reading speed of 25 % of the participating subjects (75 wpm) compared to a 20 minute instruction (23 wpm).36 Hyperocular lenses are preferred to a screen reader for the described eccentric visual training because they are mobile, even if the test subjects must first get used to the necessary shortened working distance, which is sometimes difficult to tolerate.23 The same problem was also evident in the clinical training in Masserberg. In relation to the training of Nilsson et al.,23 it is discussed that it is unclear which improvement is due to the aids used and which can be attributed to the training. In their study, the worse eye of the TS was used for the training trial to exclude pre-existing training effects on the better eye. In comparison, Nguyen et al.21 showed a further increase in reading speed of 20 wpm in patients with juvenile macular degeneration (e. g., Mb. Stargardt) who were already using a good PRL, in conjunction with optimal visual aid use. A similar increase in reading speed (+ 14 wpm) was found with additional training of AMD patients who had previously got used to their own magnifying aids for 6 weeks.28 Based on their experience, Kuester-Gruber et al.37 claim that an increase in reading speed of 10 wpm is already clinically relevant, as it was accompanied by a subjective improvement (Impact of Vision Impairment Questionnaire (IVI)). To assess clinical relevance, the increase in reading speed should be considered in relation to the baseline value. An increase of 10 wpm at a reading speed of 40 wpm at baseline should be considered higher than at > 100 wpm at baseline.38
When providing aids or training, it is important to consider the variables influencing reading speed. From the available studies with different subject collectives (mean visual acuity 0.04, reading speed of 9.8 ± 5.8 wpm 23 up to a visual acuity of 0.1 – 0.25, reading speed 83 and 102 wpm 21, respectively), it can be assumed that faster and possibly higher training successes can be achieved with better initial conditions. This applies, for example, to already established PRL and the safe use of optimally fitted magnifying aids, to which an already good reading speed can be attributed.28 It is assumed that, depending on the aid and the necessary magnification requirement for a task, more fatigue can also be expected. For example, with a magnification requirement of 6x, screen readers are more relaxed to use than optical magnifiers. In training, TS 2 got tired quickly, possibly due to the high optical magnification required. In comparison, TS 1, with already optimal aid and habit, showed hardly any difficulties in implementing the training instructions and quickly overcame the instabilities that were still present at the beginning. For both TS, the shortened working distance was a seemingly insurmountable obstacle. Thus, external motivation seems to be mandatory to successfully continue or complete eccentric vision training. Although time was not accurately measured for the TS in clinical training, it is apparent that the increased magnification requirement results in a generally slower reading speed (font size 26, Verdana – TS 1: approx. 1 minute; TS 2: approx. 20 minutes).23,28 Apparently, the font also influences the reading speed.26 However, the current knowledge on the effect of fonts seems unclear, as different fonts are favoured differently.31 In mild to moderate visual impairment due mostly to cataract and glaucoma (EDTRS visual acuity binocular approx. ≥ 0.2 to 1.6), font has little influence on reading speed. It is recommended that font size be increased from the minimum size of 10 points to 14 or 16 points to allow more people to read fluently.39 To select and use inclusive fonts, it is recommended to research the website https://www.leserlich.info/index.php. The advantage of this type of eccentric vision training is that the exercise materials can be created by the trainer without further technical effort. However, for this reason, the variation possibilities and fast flexibility during the training are limited. It is therefore an area where the use of software could be advantageous. Since the same text was always used in one font size (e. g., board 8 always in font size 26), memorisation cannot be ruled out. Limitations also arise because, instead of hyperocular lenses, we used refraction lenses (up to 24 D), which create artificial tunnel vision. In addition, the exercise texts were difficult to illuminate, especially at shorter test distances. In some cases, there were strong reflections on the exercise slides, or a shadow was cast, which made reading more difficult. However, the training with the IReST slides allows backward saccades in case of difficult recognition or difficulties with text comprehension and enables saccade planning. Due to the many individual parts of the training, it was impossible to obtain exact time measurements, which is why the evaluation of improvement in reading speed was based solely on the subjective evaluation of the therapist. Some of these limitations can be easily remedied: for example, by setting up an ergonomic training area with adapted lighting and creating multiple texts
in one font size.
Another hurdle was the motivation of the test subjects. Similar to learning a language or a sport, learning a new reading strategy requires intensive cooperation and high motivation of the TS. If they do not practise at home or do not do it sufficiently and if the TS is impatient, the clinical practice sessions alone will not be sufficient to achieve an improvement in reading speed. This must be communicated clearly to the TS. In practice, there is then also the possibility of adapting technology for the blind (e. g., reading devices, speech output, special software, or similar talking mobile aids).
With regard to training intensity, it is debated to what extent a training strategy, such as RSVP, actually ensures an improvement in reading speed or whether other components that are crucial in reading are also unconsciously improved by daily practice.28 It is also questionable to what extent it is sufficient to determine reading speed and not better text comprehension to describe the success of training.
Conclusion
Eccentric vision training or software-assisted reading training can be used in addition to an optimal supply of magnifying aids for patients with central scotoma. Considering the limitations of “manual” training, it is possible to sensitise and strengthen a compensatory, eccentric gaze deflection of the patient by simple means. At the Regiomed rehabilitation clinic in Masserberg, an additional oculomotor training will take place in the future with the microperimeter MP-3 of the company Nidek, which also works with acoustic feedback (= biofeedback) (continuous tone when steadily using the PRL / TRL). Although the small sample in the present case study could not show any direct success, it can be stated that eccentric visual training can work without complex technology. A related study with a larger number of subjects would be suitable in this context.
Images: Copyright by Johanna Lahne & Kathleen S. Kunert
Conflict of interest
The authors have no conflict of interest with respect to the methods and devices mentioned in the article.
